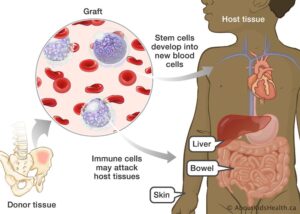
Osteoporosis is a condition characterized by the degeneration and weakness of bone tissue. Over time, osteoporosis might progress. This can lead the bone to become progressively porous and more brittle (as the disease’s name suggests). When seen under a microscope, healthy bone resembles a honeycomb. When osteoporosis is prevalent, the honeycomb’s holes and crevices appear significantly larger than in healthy bones.
Osteoporosis increases the likelihood of fractures, especially in the hips, spine, and wrists. In reality, over nine million fractures are caused annually by osteoporosis worldwide.
Causes
Osteoporosis is the most prevalent bone disorder.
Osteoporosis raises the risk of bone fracture. Approximately half of all women over the age of 50 will experience a fracture of the hip, wrist, or vertebra (spine bones) during their lifetime. Fractures of the spine are the most prevalent.
The minerals calcium and phosphate are required for the formation and maintenance of healthy bones.
- Throughout one’s lifetime, the body continues to both reabsorb old bone and produce new bone.
- As long as the body maintains a healthy balance of new and old bone, the bones remain healthy and powerful.
- Bone loss occurs when the resorption of old bone exceeds the formation of new bone.
- Sometimes, bone loss occurs for no apparent reason. Occasionally, bone loss and thin bones are inherited. In general, elderly white women are most prone to experience bone loss.
Anything that causes the body to destroy too much bone or prevents it from producing enough new bone can result in brittle, fragile bones. Instead of retaining calcium and phosphate in the bones as you age, your body may reabsorb these minerals. This causes bone weakness.
Who suffers from osteoporosis?
Osteoporosis is more prevalent in elderly women, particularly women of non-Hispanic white and Asian descent. Nevertheless, it can occur at any age, in both men and women, and across all ethnic groups. People over the age of 50 have the highest chance of acquiring osteoporosis and fractures associated with it. One in two women and one in six men over the age of 50 may experience an osteoporosis-related fracture at some point in their lives. Over the age of 50, approximately 4.5 million women and 0.8 million men in the United States suffer osteoporosis.
However, an additional 22.7 million women and 11.8 million men over the age of 50 suffer from reduced bone mass (known as osteopenia). Those with poor bone mass are also at a greater risk for fractures, though not as much as those with osteoporosis. If bone loss persists, individuals with osteopenia can develop osteoporosis.
Risk factors associated with osteoporosis
These risk factors cannot be modified:
- Being older than 70 years
- Being female
- Having fallen previously
- Your parents’ history of hip fractures
- Premature menopause
Among the risk factors that can be mitigated are:
- Lack of physical activity
- Weak muscle bulk and power
- Low body mass index (BMI) less than 20kg/m2)
- Smoking
- Excessive alcohol intake
- Insufficient consumption of energy-dense meals and proteins.
Certain illnesses increase the likelihood of developing osteoporosis. These consist of:
- Hypogonadism and precocious menopause
- Bone-wasting diseases, such as rheumatoid arthritis
- Hyperthyroidism or hyperparathyroidism
- Chronic illness of the liver or kidneys
- Celiac and inflammatory bowel diseases
- Cushing’s disease
Certain drugs can also raise your risk of developing osteoporosis:
- Steroids used for more than three months
- Anti-androgen therapy – medicines that prevent testosterone from functioning and are occasionally used to treat prostate cancer
- Aromatase inhibitors – medications used to treat or prevent ovarian or breast cancer that restricts the production and action of estrogen.
- Long-term usage of thyroid hormone replacement treatment, which can be a risk factor
- Antidepressant medications, especially those belonging to the SSRI class.
- Proton pump inhibitors — medications that reduce gastric acidity
- Thiazolidinedione – a drug used occasionally to treat diabetes
- Antipsychotic drugs – some pharmaceuticals used to treat mental disorders including schizophrenia
- Anti-epileptic drugs – some drugs used to control epilepsy
Diagnosis
If you have osteoporosis risk factors, it is imperative that you request a bone health evaluation from your doctor.
As part of a ‘check-up’ on your bone health, your doctor should obtain a comprehensive medical history, including details on any recent fractures. In addition, your doctor will likely predict your future fracture risk using an instrument like FRAX®.
A Bone Mineral Density (BMD) test may be recommended based on the results of your fracture risk assessment. In some countries (e.g., the United States), BMD testing is advised for all 65-year-old women and men, regardless of risk factors.
What does a bone mineral density (BMD) test measure?
BMD testing is a safe, quick, and painless way to determine if you have osteoporosis or are at risk of developing it in the future.
Traditional X-rays used to detect damaged bones (such as spine fractures) cannot quantify bone mineral density (BMD). BMD requires more specific techniques for measurement. DXA (dual-energy X-ray absorptiometry), which stands for dual-energy X-ray absorptiometry, is the most popular and approved BMD test. DXA is an X-ray that can identify fairly modest percentages of bone loss.
What do my DXA findings indicate?
The T-score on your bone density assessment indicates the degree to which your bone mass deviates from that of a typical healthy adult in their twenties.
The T-score is assessed in standard deviations (SD) and indicates if your bone mass is within the normal range, if you have osteopenia (a stage of bone loss between normal bone density and osteoporosis), or if you have osteoporosis (a T-score of -2.5 or lower).
BMD test results (osteoporosis T score) | |
Status | Hip BMD T-score (SD) |
Normal | -1 and above |
Osteopenia (low bone mass) | Between -1 and -2.5 |
Osteoporosis | -2.5 or lower |
Severe Osteoporosis | -2.5 or lower and the presence of at least one fragility fracture |
Pregnancy and Lactation Associated Osteoporosis (PLO)
Temporary losses in bone density are a natural occurrence during pregnancy and lactation, however fractures are relatively uncommon during this time.
Fractures of the spine are most frequently associated with severe back pain, but PLO can also be associated with hip fractures and other types of fractures.
PLO is often diagnosed when a pregnant or lactating woman suffers acute back pain and imaging indicates multiple vertebral fractures.
Some women with PLO have been diagnosed with osteoporosis prior to pregnancy, but the majority of women with PLO have never been diagnosed with osteoporosis and have never undergone a bone evaluation prior to the onset of symptoms.
Treatment for Osteoporosis
The objectives of osteoporosis treatment are to halt or stop bone loss and avoid fractures. Your medical professional may suggest:
- Adequate nutrition
- Lifestyle modifications
- Exercise
- Prevention of falls to prevent fractures
- Medications
People who acquire osteoporosis as a result of another condition should work with their physician to determine and treat the underlying cause. For instance, if you are using a medicine that causes bone loss, your doctor may reduce your dosage or switch you to a different prescription. If you have a condition that requires long-term glucocorticoid therapy, such as rheumatoid arthritis or chronic lung disease, you can also take approved drugs for the prevention or treatment of osteoporosis linked with age or menopause.
Your therapy will depend on your specific condition; you should discuss this with your physician. Among the treatments available are:
- Calcium and vitamin D (alendronate, risedronate, ibandronate, etidronate, zoledronate)
- The compounds Teriparatide and parathyroid hormone
- Raloxifene
- Calcitonin
- Denosumab
- Strontium ranelate
- Replacement hormone therapy (HRT).
Pain management
Everyone experiences pain differently, so what is effective for you may not be effective for someone else.
There are numerous pain management options, including:
- Painkillers
- Heat therapy, including warm baths and hot packs
- Cold therapy, such as ice packs
- Transcutaneous electrical nerve stimulation (TENS) – this is believed to alleviate pain by activating nerves.
- Simple relaxation techniques
- Massage
- Hypnosis
You can employ multiple approaches at once to control your pain; for instance, you could combine medication, a hot pack, and relaxation techniques.
Preventing osteoporosis
Diet
To maintain strong, healthy bones throughout life, a calcium-rich diet is required. One cup of nonfat or one percent milk contains 300 mg of calcium.
Salmon with bones, sardines, spinach, broccoli, calcium-fortified beverages and bread, dried figs, and calcium supplements are other sources of calcium. The finest sources of calcium are foods and beverages.
Remember that the body can only absorb 500 mg of calcium at a time if you require supplements. Calcium supplements should be taken in divided dosages, as anything beyond 500 mg will not be absorbed.
Vitamin D is also essential because it enables calcium absorption in the body. Below are the recommended daily intakes of vitamin D. Milk fortified with vitamin D can also be obtained by sun exposure a few times per week.
Lifestyle
A healthy lifestyle helps lessen the severity of the bone loss. Begin a regular workout routine. Walking, jogging, aerobics, and weightlifting are the best exercises for bone strength because they force your muscles to work against gravity.
Do not consume excessive alcohol. Avoid consuming excessive quantities of caffeine. Never use tobacco products.
Preventing falls
By implementing a few easy changes at home, the chance of breaking a bone in a fall can be reduced.
Check your home for any tripping risks, such as trailing cables. Ensure the stability of rugs and carpets, and use rubber mats at the sink and in the bathtub to prevent slipping.
Have frequent vision and hearing exams. Some elderly individuals may need to wear hip guards to absorb the impact of a fall. Your primary care physician can offer assistance and guidance regarding changes to your lifestyle.