Crohn’s disease is a chronic bowel ailment that produces inflammation in the gastrointestinal tract and can result in stomach pain, diarrhea, weight loss, and malnutrition. The digestive system can be affected by Crohn’s disease from the mouth to the anus.
Currently, the cause of Crohn’s disease is unknown. Having a close relative with an inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis) may increase your risk.
Crohn's disease causes
Immune system
It indicates that activation of the immune system in the intestines has a significant role in IBD. In the absence of any identifiable intruder, the immune system is inappropriately and chronically activated in IBD patients. This leads to persistent inflammation and ulceration.
Genetics
The propensity to aberrant immune system activation is inherited genetically. Therefore, first-degree relatives (brothers, sisters, children, and parents) of individuals with IBD are more prone to develop these conditions. Recently, the NOD2 gene was discovered to be related with Crohn’s disease. This gene plays a crucial role in determining how the body reacts to certain bacterial products. Individuals with gene mutations are more likely to acquire Crohn’s disease.
Other genes, such as autophagy related 16-like 1 gene (ATG 16L1) and IRGM, which both contribute to macrophage abnormalities and have been identified through the Genome-Wide Association study, are currently being identified and explored as being crucial to understanding the pathophysiology of Crohn’s disease.
Bacteria
There are increased numbers of a certain type of bacterium, E. coli, in the intestines of persons with Crohn’s disease, which may have a role in the disease, according to research. A genetically determined impairment in the clearance of E. coli by intestinal mucosal macrophages is one of the hypothesized mechanisms by which this could occur. The precise roles played by each of these elements in the development of this disease are unknown.
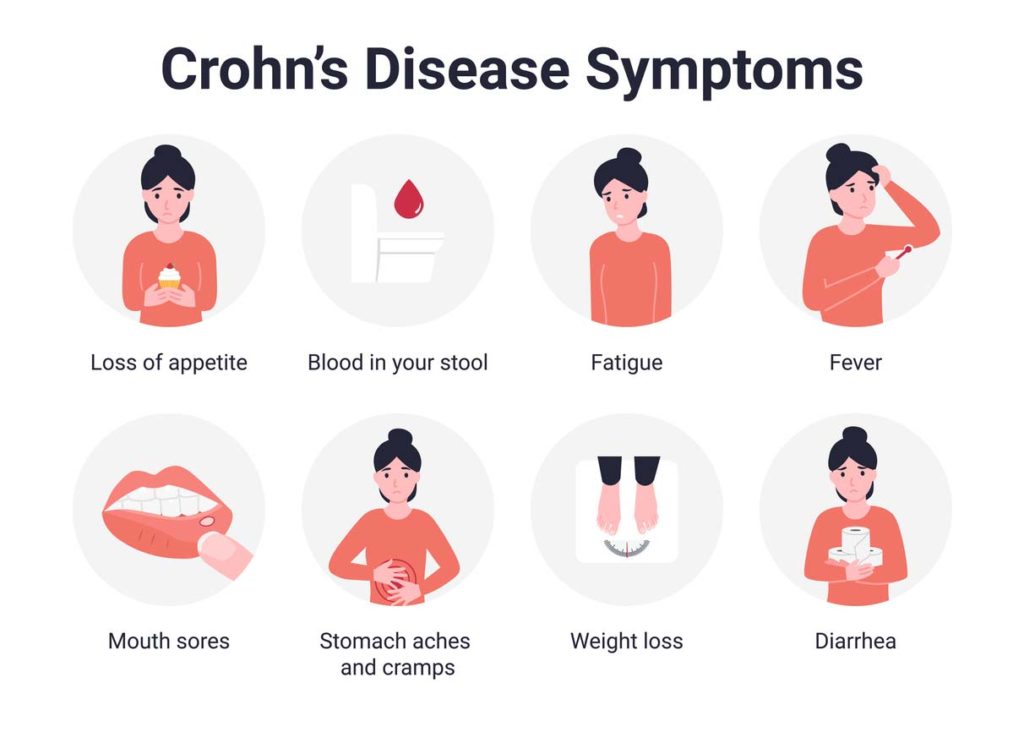
Crohn's disease symptoms
Symptoms depend on the affected portion of the digestive tract. The severity of the symptoms ranges from mild to severe, and flare-ups might occur intermittently.
The principal Crohn disease symptoms are:
- Abdominal cramping pain (belly area).
- Fever
- Fatigue
- Appetite loss and weight loss.
- The sensation of needing to defecate when the bowels are already empty. It may involve exertion, discomfort, and cramps.
- Diarrhea that is watery and may be bloody.
- Other possible symptoms include:
- Constipation
- Sores or inflammation of the eyes
- Drainage of pus, mucus, or feces from the region of the rectum or anus (caused by something called a fistula)
- Joint discomfort and enlargement
- Oral ulcers
- Rectal hemorrhage and bloody feces
- Swollen gums
- Sore, crimson lumps (nodules) beneath the skin that may develop into skin ulcers
Diagnosis
To diagnose Crohn’s disease or colitis, we begin with a complete physical examination and medical history. Several diagnostic tests are required to confirm a diagnosis. They may consist of:
- Colonoscopy and flexible sigmoidoscopy: These diagnostic procedures employ a thin, flexible tube equipped with a camera to inspect the colon, small intestine, and large intestine for ulcers, bleeding, and inflammation.
- Upper endoscopy: A thin, flexible tube equipped with a camera is placed through the mouth and followed down the gastrointestinal tract to the stomach and upper small intestine in search of bleeding, ulcers, and inflammation.
- Capsule endoscopy: The patient swallows a capsule with a camera to capture images of areas of the digestive tract that are difficult to access with other techniques (capsule passes normally in the stool).
- Laboratory examinations include blood tests and stool samples to detect bacteria and intestinal hemorrhage.
- CT interography and MR interography: Specialized radiology studies that assess the small intestine, a region of the gastrointestinal tract that colonoscopy and upper endoscopy cannot reach, but where Crohn’s disease is frequently present.
- Imaging tests: Collaborating with experts in Radiology for imaging and interpreting gastrointestinal abnormalities, such as abdominal x-rays, barium enema, computed tomography (CT scan), fistulogram (to assess fistulas in patients with Crohn’s disease), and MRI.
Crohn's disease treatment
Despite the fact that there is no cure for Crohn’s disease, medication can help minimize the condition’s impact on your life. Your physician or expert may also recommend a diet tailored to your condition.
Vitamin supplements
If you have difficulty absorbing nutrients owing to inflammation in the small intestine, you may be susceptible to vitamin shortages. If this is the case, your physician, nutritionist, or IBD nurse will advise you to take a vitamin supplement. The most typical shortcomings include:
Iron deficiency can cause anemia, a condition in which there is a shortage of hemoglobin or red blood cells that carry oxygen throughout the body. Iron supplements may be administered orally or intravenously through a vein in your arm.
Calcium – steroid use can lead to calcium loss and osteoporosis. Vitamin D and calcium supplements may help avoid this. Learn more in Bones.
Vitamin B12 – Individuals who have had the final portion of their small intestine removed or who have inflammation in that region may not be able to absorb this vitamin. This can result in a type of anemia that is treated with vitamin B12 injections.
Vitamin D is essential for a healthy immune system and strong bones. When the skin is exposed to sunshine, the body produces vitamin D. It can also be obtained by the consumption of oily fish, egg yolks, and foods fortified with vitamin D, such as margarine and breakfast cereals. People with Crohn’s disease are more prone to have low vitamin D levels. A recent study indicates that low vitamin D levels may raise the likelihood of Crohn’s flare-ups; however, it is unclear whether low vitamin D levels induce flare-ups or are the result of them.
Medications
Crohn’s disease is characterized by times of “relapse” when inflammation in the intestine flares up and periods of “remission” when inflammation subsides. The purpose of treatment is to address relapses when they occur and to allow the bowel to repair. In addition, medications are used to sustain remission, enhance general health, and avoid the development of problems.
Common anti-inflammatory medications used to treat Crohn’s disease include:
- Steroids
- Aminosalicylates to control relapse frequency
- Immunosuppressant medications
- Antibiotics
You may also be instructed to take medications to treat diarrhea, alleviate pain, and supplement your diet (for example, to boost your iron levels, vitamin D, and calcium).
Surgery
Surgery for Crohn’s disease can remove or enlarge severely diseased parts of the intestine. Typically, the healthy ends of the bowel are reconnected.
If the condition is really severe, a stoma (an artificial opening in the stomach that diverts feces or pee to a bag) may be necessary. It’s normal to feel apprehensive about the prospect of living with a stoma, but it can significantly enhance a person’s quality of life.
Being affected by Crohn’s disease
Most persons with Crohn’s disease are able to enjoy life, including jobs, travel, recreation, sex, and having children, with proper management.
To maintain your health, consider
- Keeping a diet journal to determine if certain foods exacerbate your symptoms during a flare-up
- Asking your physician about nutritional supplements if you suspect malnutrition
- Give up smoking if you have Crohn’s disease and are a smoker. There is evidence that smoking can exacerbate and make it more difficult to manage Crohn’s disease.
- Regular exercise to improve your mood and reduce stress
- Learning relaxing techniques to assist with stress management
Complications
The risk of consequences is increased if symptoms are strong and frequent. Any of the following issues may necessitate surgery:
Internal hemorrhage
- A stricture occurs when a portion of the intestine becomes constricted, resulting in the formation of scar tissue and partial or total obstruction of the intestine.
- A perforation is a small hole in the intestinal wall that can result in leaking, infections, and abscesses.
- Fistulas, involve the formation of a canal between two sections of the gut
Moreover, a person may have:
- A chronic iron deficiency
- Food digestion issues
- Slightly increased risk of colon cancer
Preventing flare-ups of Chron's disease
There is no prevention for Crohn’s disease. These healthy lifestyle modifications help lessen symptoms and flare-ups:
- Stop smoking
- Consume a nutritious, low-fat diet
- Exercise regularly
- Manage stress
Being affected by Chron's disease
- Living with Crohn’s disease might be challenging at times, but there’s no reason you can’t lead a normal life if your symptoms are effectively managed.
- Adults with Crohn’s disease do not require a specific diet, but children may require a particular liquid diet to control their symptoms. Aim for a balanced, healthful diet.
- Some individuals report that particular meals seem to exacerbate their symptoms.
- Whether you suspect a specific meal is causing your symptoms, see if avoiding that food helps.
- However, before making any changes to your diet, consult your doctor or care team.