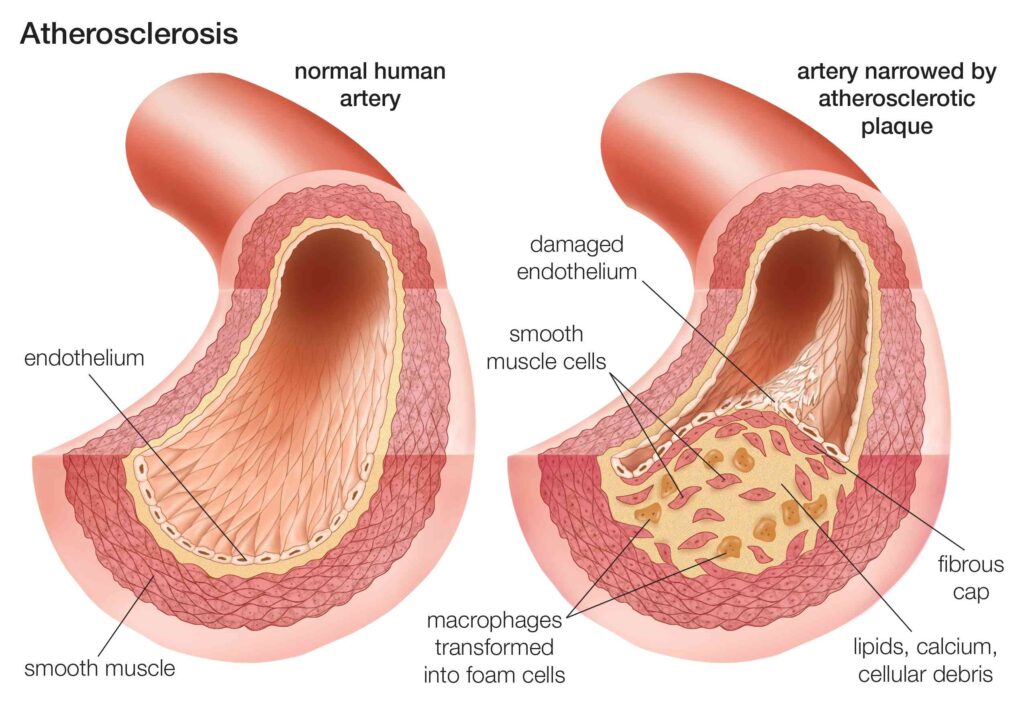
Arteriosclerotic heart disease (ASHD) is characterized by a thickening and hardness of the coronary artery walls. Atherosclerosis (a type of arteriosclerosis) is a potentially fatal disorder in which arteries get blocked with fatty plaques or atheroma.
Diabetes is associated with an increased risk of developing atherosclerosis. Cardiovascular events such as myocardial infarction, stroke, peripheral vascular disease, and mortality are elevated by a factor of two or three when compared to the general population. This risk is up to tenfold greater in premenopausal women since they lose their usual protection against cardiovascular disease.
Facts about coronary artery disease
Atherosclerosis is directly or indirectly linked to coronary artery disease (CAD). The top facts are:
- Around 18 million adults in the United States aged 20 and older have heart disease.
- Each year, more than 800,000 Americans have a heart attack.
- Each year, around 650,000 Americans die of heart disease.
- Coronary heart disease accounts for around 25% of fatalities in the United States.
- Half of all men have severe atherosclerosis without experiencing any symptoms.
- Men die of coronary artery disease at a higher rate than women. Women’s rates increase after menopause but never catch up to men’s.
- Heart disease is the leading cause of death in both men and women.
Risk factors of developing atherosclerosis
The risk factors are divided into major and minor risk factos.
Major risk factors
Unmodifiable
- Increasing age (atherosclerosis is more common as people get older)
- Gender (At younger ages, males are more at risk. Premenopausal women are relatively protected; after menopause, the risk in women increases and eventually exceeds the risk in males.)
- Family history
- Genetic abnormalities (lots of these probably exist; many aren’t fully understood).
Modifiable
- Hyperlipidemia (best thing to do is have a high level of HDL cholesterol, which actually scavenges lipids and removes them from atherosclerotic plaques, and a low level of LDL, which is the “bad” cholesterol that makes up part of the plaques.
- Hypertension (there’s no one right number, but it should be at least below 140 systolic and 90 diastolic)
- Cigarette smoking (smoking potentiates the other risk factors)
- Diabetes (patients with diabetes mellitus have an increased amount of atherosclerosis at a younger age)
- C-reactive protein level (this is a serum marker of inflammation; the higher the level, the greater the risk for atherosclerosis)
Minor risk factors
- Obesity
- Inactivity on the physical front
- Stress
- Estrogen insufficiency postmenopausal
- Consumption of a lot of carbohydrates
- Lipoprotein (an altered form of LDL that seems to be independently associated with increased risk of atherosclerosis)
- Consumption of trans fats
- Infection with Chlamydia pneumoniae (Chlamydia pneumoniae and other bugs have been discovered in plaques but not in normal arteries, and individuals with more severe atherosclerosis had higher antibody titers to C. pneumoniae. However, no causal relationship has been shown.)
ASHD symptoms
Symptoms of CAD are not noted until the artery is significantly damaged. Severe artery damage decreases blood flow to the heart, which presents as:
- Angina or chest pain that spreads across the chest
- Shortness of breath
- Heart attack is experienced if the coronary artery is completely blocked
- Other associated symptoms include:
- Nausea
- Sweating
- Fatigue
- Faster heartbeat
- Weakness or dizziness
Diagnosing ASHD
Diagnostic testing may include the following:
- Electrocardiograph (EKG) tests: This procedure records the heart’s electrical activity. Can be used to detect heart attacks, ischemia, and abnormal heart rhythms.
- Exercise stress tests: This is a treadmill test that determines how well your heart performs under duress. Can be used to detect angina and coronary occlusions.
- Rather than employing exercise to stress your heart, medication is given to boost your heart rate and stimulate activity. This test is capable of detecting angina and coronary occlusions.
- Coronary calcium scan: This test determines the calcium content of the walls of your coronary arteries, which can be an indication of atherosclerosis.
- Echocardiogram: This test uses sound waves to determine the health of your heart’s architecture and overall function.
- Numerous blood tests are conducted to assess factors affecting the arteries, including triglycerides, cholesterol, lipoprotein, C-reactive protein, glucose, and HbA1c (a measure of diabetes management).
- Cardiac catheterization is a procedure that involves inserting tiny tubes into the heart’s blood arteries to assess heart function and the existence of coronary artery disease.
- Additional diagnostic imaging studies may include the following:
- Nuclear imaging: After delivering a radioactive tracer, this technique produces images of the heart.
- Computed tomography angiogram: This procedure uses CT and contrast dye to create three-dimensional images of the beating heart and to locate coronary artery blockages.
ASHD treatment
Medical treatment
Aspirin: Aspirin works by decreasing your chance of developing a blood clot. Blood clots in the coronary arteries can result in a potentially fatal heart attack Additionally if you’ve previously had a heart attack, this medicine may help prevent future ones. However, if you have a bleeding issue or if your doctor has already recommended another blood thinner, you should avoid taking aspirin.
Medication to lower cholesterol: These drugs help to lower blood pressure and inflammation. They include statins. Improving your cholesterol level can help prevent the formation of plaque, partially reverse existing plaque deposition, and reduce artery irritation.
Beta-blockers: These drugs cause a decrease in heart rate. As a result, your heart is less required to work as hard and has more time to “relax.” This reduces your heart’s oxygen need. Additionally, these drugs are useful for treating arrhythmias.
Calcium channel antagonists: Occasionally, a beta-blocker alone is insufficient to lower your blood pressure. In this scenario, your physician may prescribe a calcium channel blocker in addition to other drugs. Maintaining a normal blood pressure level also reduces the risk of stroke or heart attack.
Additional drugs: Along with calcium channel blockers, your doctor may prescribe other drugs to help relieve chest discomfort or angina. Ranolazine (Ranexa) and nitroglycerin are two examples (Rectiv). Additionally, angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers or diuretics are used to reduce blood pressure.
Surgical options
Angioplasty, alternatively referred to as percutaneous transluminal coronary angioplasty or PTCA, is a procedure that involves introducing a long flexible tube called a catheter into a blood vessel via a small incision in the skin. The catheter’s tip is deflated. Once the catheter reaches the blocked blood vessel, the balloon is inflated and the plaque is compressed against the blood vessel’s walls. The balloon may be repeatedly inflated and deflated.
Frequently, the treatment is performed in conjunction with the placement of a thin metal tube called a stent in the artery to act as a scaffold, keeping the artery open and preventing the plaque from springing back toward the vessel’s core.
Rotary atherectomy opens restricted arteries by “sanding” away plaque with a high-speed rotational instrument. This procedure is employed in specific circumstances, such as with plaque with a high calcium content or to widen blockages within a stent.
A coronary stent is a tiny, latticed, high-grade stainless steel tube used to keep the coronary artery open following angioplasty. It is inserted into the coronary artery in the same way as angioplasty is. Typically, the stent is placed in the constricted section of the artery. When the balloon on the catheter is inflated, the stent expands and contacts the vascular wall. The balloon is deflated and removed, leaving the stent in place permanently.
Following stent placement, you will be prescribed an antiplatelet medicine for one month, Clopidogrel, popularly known as Plavix. This technique is intended to reduce the danger of clot development within the stent while tissue grows around it to integrate it into the blood artery wall. Within a month, the body loses awareness of the stent and the drug is no longer required. You should continue to take aspirin in addition to the Clopidogrel if prescribed.
Coronary artery bypass graft (CABG) surgery is a procedure in which an artery or vein from another part of the body is connected to the blood vessel in order to redirect blood around the obstruction. Traditionally, this is accomplished with open-heart surgery. The surgeon makes a big incision across the breastbone to gain access to the heart; during part of the surgery, your heart will be halted and a heart-lung machine will be used to pump your blood and assist you in breathing.
UCSF offers a minimally invasive bypass surgery alternative in which the surgeon gains access to the heart through a small incision rather than cutting bones. There is no need to stop your heart, and the majority of patients do not require heart-lung bypass. The recuperation period is between ten and two weeks, as opposed to the three to four months required for open-heart bypass surgery. In the Western world, CABG is the most effective and frequently performed major heart surgery.