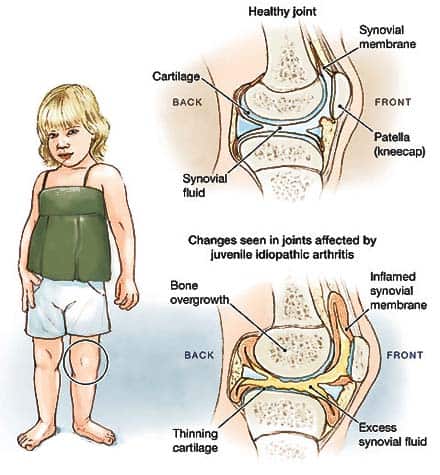
Juvenile idiopathic arthritis (formerly known as systemic juvenile rheumatoid arthritis) is an umbrella term encompassing adolescent rheumatic disorders that begin before the age of 16 and are defined by joint inflammation that lasts for more than six weeks. On the basis of the pattern of joint involvement, the existence of extra-articular symptoms (such as uveitis, rash, nail changes, lymphadenopathy, and hepatosplenomegaly), laboratory findings, and illness prognosis, it is categorized into distinct kinds. Oligoarticular JIA, the most prevalent form, is characterized by asymmetric involvement of up to four joints (with the knee joint most often affected). Nearly half of all instances with oligoarticular JIA are accompanied by anterior uveitis, which can be identified via a slit-lamp examination. Classification and prognosis of JIA are determined by laboratory testing including ESR, rheumatoid factor (RF), antinuclear antibodies (ANA), and the HLA-B27 antigen test. Similar to adult rheumatoid arthritis, juvenile idiopathic arthritis is treated with nonsteroidal anti-inflammatory medicines (NSAIDs), intra-articular steroid injections, and disease-modifying antirheumatic drugs (DMARDs) such as methotrexate. A systemic glucocorticoid regimen should be avoided due to the danger of stunted growth.
Symptoms of systemic juvenile rheumatoid arthritis
The symptoms of juvenile rheumatoid arthritis may manifest in episodes (flare-ups) or be persistent and chronic. These are the most prevalent manifestations of juvenile rheumatoid arthritis. However, each child’s symptoms may manifest differently. Possible symptoms include:
- Swollen, rigid, and painful joints, particularly in the morning or following a nap (joints in the knees, hands and feet are most commonly affected)
- Reduced usage of one or more specific joints
- Fatigue
- High temperature and redness, if juvenile systemic rheumatoid arthritis
- Lymph node enlargement, if juvenile systemic rheumatoid arthritis
- Eye irritation (especially ANA positive pauciarticular disease)
- Reduced appetite, poor weight gain, and sluggish development
The symptoms of juvenile rheumatoid arthritis may resemble those of other diseases or disorders. Consult your child’s physician for a diagnosis at all times.
Causes of JIA
All forms of JIA occur when the immune system, which normally assaults pathogens, attacks the joints instead. This results in joint inflammation (swelling and irritation) and other complications.
Systemic JIA can manifest in children aged 1 to 16 at any time. The majority of instances begin at 2 years of age. The disorder equally affects boys and girls.
Doctors do not know the specific cause of JIA in children and adolescents. Idiopathic implies “of uncertain origin.” It can run in families, but this is uncommon. It’s probably a combination of:
- Inherited (genetic) causes
- The manner in which the immune system reacts to infection and disease
- A catalyst, like an infection
Classification
Classification based on symptomatology (according to the International League of Rheumatology Associations):
- Oligoarticular JIA:
- Arthritis affecting less than five joints
- Additional subdivisions:
Persistent oligoarthritis: patients with 1–4 afflicted joints who do not develop arthritis in 5 or more joints within the first six months of illness onset.
Extended oligoarthritis: patients with 1–4 afflicted joints who develop arthritis in more than 4 joints within the first six months of illness onset.
- Polyarticular JIA:
Arthritis in fewer than five joints
Additional subdivisions:
Positive Rheumatoid factor (RF) for polyarthritis
Polyarthritis with negative RF
- Systemic JIA (formerly known as Still’s disease):
Arthritis of one or more joints
Fever lasting 2 weeks and occurring every day for at least 3 days
A minimum of one of the following:
- Exudative, erythematous rash
- Hepatomegaly
- Splenomegaly
- Lymphadenopathy (LAD)
- Serositis
- JIA Psoriatic:
- Enthesitis arthritis (also referred to as pediatric spondyloarthropathy):
- Display symptoms of arthritis and enthesitis (inflammation of the entheses, the sites where tendons or ligaments insert into the bone)
- May only manifest with arthritis or enthesitis and two of the following criteria:
- Sacroiliac (SI) joint tenderness or lumbosacral pain related to inflammation
- Positive HLA-B27 Antigen
- First-degree relative affected by acute anterior uveitis, ankylosing spondylitis, inflammatory bowel disease (IBD) with sacroiliitis, or reactive arthritis.
JIA without differentiation:
Patients who fit requirements for many categories
Patients who do not fulfill all of the requirements for another category
Diagnosing systemic juvenile rheumatoid arthritis
Since there are no diagnostic tests for JIA, the physician will attempt to rule out alternative causes of arthritis and other diseases as the origin of the symptoms.
To diagnose JIA, the physician will collect a thorough medical history, including a description of symptoms, and conduct a physical examination. In addition, the physician will examine the joints for signs of arthritis.
These tests may also be ordered by a physician:
- Imaging techniques such as X-rays or magnetic resonance imaging (MRI) to determine the state of the joints;
- Blood, urine, and/or joint fluid laboratory testing to assist determine the kind of arthritis. These include the determination of the level of inflammation and the presence of antinuclear antibody (ANA) and rheumatoid factor. These tests can also help rule out other diseases — such as an infection, a bone issue, or cancer — or an injury as the underlying cause of the symptoms.
Treatment
To minimize symptoms and avoid joint degeneration, JIA treatment focuses on addressing the underlying inflammation. Treating the inflammatory response might also aid in the improvement of rashes.
Various drugs can aid in the management of JIA symptoms, such as:
- Nonsteroidal anti-inflammatory medications are often the first-line treatment for minor pain prescribed by physicians.
- Oral corticosteroids: These medications aid in the reduction of systemic inflammation in mild to severe diseases.
- Corticosteroids administered intravenously: These medications reduce inflammation in patients with severe illness and those with consequences, such as MAS.
- Disease-modifying antirheumatic medications: These treatments help stop or delay the progression of inflammatory forms of arthritis.
- Inflammatory cytokine blockers: These medications reduce inflammation. An example is anakinra. Another is canakinumab.
Complications
Biologic drugs have been found to have a rather favorable safety profile for children in terms of medical treatment-related consequences. Despite studies suggesting an increased incidence of lymphoproliferative cancers in children receiving biologic medicines, a true causal association has not been shown (Hay, 2012). As previously noted, the surgical therapy of joint disease in systemic JIA presents substantial complications.
The most feared consequence of systemic JIA is macrophage activation syndrome, with a death incidence of up to 20%. (Hay, 2012). The body creates an excessive anti-inflammatory response due to the overactivation and proliferation of T cells and macrophages. Macrophage activation syndrome is characterized by prolonged fever, hepatosplenomegaly, liver dysfunction, changes in mental status, lymphadenopathy, cytopenia, mucosal bleeding, and purpura. Renal and respiratory failure, hypotension, and shock can develop in extreme situations (Hay, 2012). The laboratory results will reveal a reduction in Vitamin-K-dependent clotting factors and a paradoxical fall in the ESR, while the CRP remains elevated. This life-threatening illness requires prompt treatment with a strong dosage of methylprednisolone (Hay, 2012).
Due to the deleterious effect of chronic inflammation on the growth hormone/insulin-like growth factor axis, 10-20% of children with any type of juvenile idiopathic arthritis will have a shorter final height. This diminution in height can also be attributed to drug use, namely the use of glucocorticoids for more than a year. Lastly, children with JIA have a decreased lean muscle mass and an increased fat mass on average (Bechtold, 2014).



