What is HOCM?
Hypertrophic Obstructive Cardiomyopathy (HOCM) is the leading cause of sudden cardiac death in the young people. A characteristic finding of HOCM is abnormal thickening or hypertrophy of the myocardium. Hypertrophy can occur in any part of the left ventricle but the inter-ventricular septum is the most common site. The interventricular septum is present between the two lower chambers of the heart. The thickened septum may reduce or even block blood flow from the left ventricle to the aorta called “outflow tract obstruction”. This requires the ventricles to pump harder to overcome the obstruction.
What are the causes of HOCM?
Hypertrophic Obstructive Cardiomyopathy is basically an autosomal dominant genetic disorder due to spontaneous mutations in the genes encoding sarcomere proteins of the contractile element of myocytes. Mutations can also occur in genes encoding for beta-myosin heavy chain or myosin binding protein C of myocardial muscle cells. Mutations in alpha-tropomyosin and troponin T have also been identified.
These mutations result in abnormally thickened myocardial cells and they lose their proper alignment and come together in a disorderly fashion. This can be described pathologically as “myocardial disarray”. Over time, fibrous tissue replaces these myocytes.
Other causes of HOCM include:
- Abnormal thickening of the coronary arteries may not remain elastic and lose the ability to dilate. This results in ischemia of the myocardial tissue, leading to ventricular fibrosis and compensatory hypertrophy.
- High blood pressure
- 3. Aging
Prevalence of HOCM
The prevalence of this disease in the general population is 1:500 which means one person in 500 has the probability of being diagnosed with HOCM. This is more than the prevalence of multiple sclerosis which affects one in 700 people. Moreover, it affects men and women equally.
HOCM symptoms
Most patients with hypertrophic obstructive cardiomyopathy remain asymptomatic throughout life. However, some patients present with the following symptoms:
- Shortness of breath
- Chest pain that occurs on exertion and physical exercise
- Fainting (syncope)
- Fatigue
- Palpitations due to abnormal cardiac rhythms such as atrial flutter and atrial fibrillations.
- Dizziness and light-headedness
- Swelling of the legs, ankles, and veins of the neck.
How to diagnose HOCM?
It is difficult to diagnose hypertrophic obstructive cardiomyopathy and can be quite challenging for health professionals. It often goes undiagnosed until a significant cardiac event occurs. We can diagnose HOCM through ECG and echocardiography. Elevated troponin is seen in HOCM but we don’t diagnose it by measuring troponin level because troponin can be elevated in many other medical conditions. Following are the characteristic findings of HOCM:
Patient examination
HOCM can be suspected if the following features are identified during patient examination along with the above-mentioned symptoms.
- Jerky pulse
- Large a wave in JVP
- Double apex beat
- Presence of fourth heart sound (S4)
HOCM is associated with Wolff Parkinson White (WPW) syndrome and Friedrichs ataxia. These patients should undergo an echocardiogram to identify any heart problem that could be present.
ECG findings
The classic finding in a patient with HOCM is left ventricular hypertrophy. This is shown on the ECG as large “septal Q waves” in the lateral and inferior leads. HOCM is a cause of long QT syndrome. Therefore, QT interval may be increased in the ECG. Right bundle branch block (RBBB), prolonged PR interval, features of left ventricular hypertrophy and non-specific T-wave abnormality can also be present. A 24 hour ECG can record the events of arrhythmias.
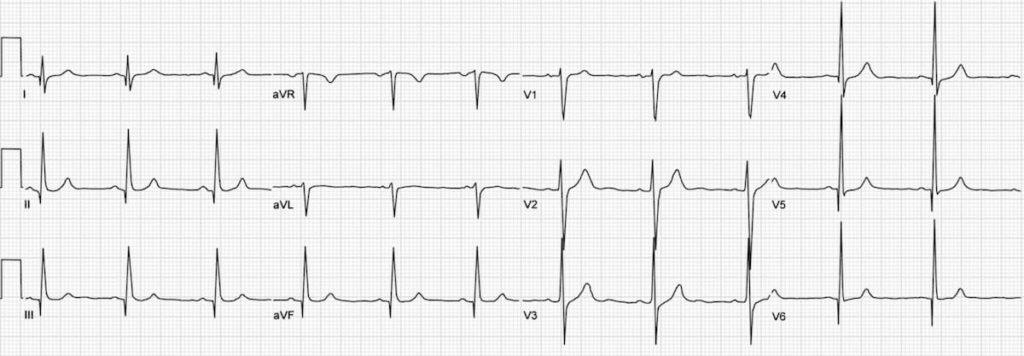
This HOCM ECG is showing
- Deep Q waves in inferior leads (I, III, aVF), and lead aVL, V5-6.
- Voltage criteria for LVH.
ECHO findings
On echocardiography, we can directly visualize the enlarged inter-ventricular septum. Doppler echocardiography can identify the extent and degree of hypertrophy and describe the presence of mid-ventricular obstruction. The classical echocardiography findings are mitral regurgitation, systolic anterior motion of mitral valve leaflet and asymmetric hypertrophy (interventricular septum thickness : left ventricular wall thickness > 1.3 : 1).
Characteristics of HOCM Murmur
We can hear a characteristic murmur on physical examination of a patient with hypertrophic obstructive cardiomyopathy. It is a mid-systolic and high-pitched murmur heard at the left lower border of the sternum. Click here to listen to: HOCM murmur.
Louder HOCM murmur
HOCM murmur becomes louder on the Valsalva maneuver. This maneuver reduces left ventricular filling resulting in reduced left ventricular outflow and thus, a decrease in preload making the murmur quiet louder.
The same effect is observed when standing from the sitting posture. This results in the pooling of blood in the legs and a decrease in venous return.
Softer HOCM murmur
HOCM murmur becomes softer when there is an increase in preload, i.e. when sitting from a standing position. This is due to increased venous return which results in the decreased intensity of the murmur.
HOCM treatment
Hypertrophic obstructive cardiomyopathy treatment depends on its severity. Mild disease can be treated with lifestyle modifications. However, moderate to severe forms of the disease require medical or surgical treatment.
Medical
Treatment aims to reduce heart rate to increase the diastolic filling time. This is because left ventricular hypertrophy in patients of HOCM obstructs left ventricular outflow during systole.
For this reason, negative ionotropic agents are given to patients to reduce the force of contraction and thus decrease heart rate. Two classes of drugs are considered for this purpose.
- Beta-blockers reduce the heart rate and have a negative ionotropic effect on the left ventricle. This provides relief against symptoms of HOCM.
- Non-dihydropyridine calcium channel blockers act in the same way as described above.
- The third line of drug treatment, disopyramide is used if beta-blockers and calcium channel blockers fail. It is an anti-arrhythmic drug but has a prominent side effect profile. It prolongs the QT intervals and causes dry mouth, reduced perspiration, urinary retention, and visual disturbances. So, disopyramide should be used simultaneously with beta-blockers or calcium channel blockers.
- Cardioverter defibrillator can be used to terminate any arrhythmia.
- Dual chamber pacemaker can be used to maintain the normal heart rate.
Drugs to avoid
The following drugs should be avoided in HOCM patients:
- ACE inhibitors
- Nitrates
- Ionotropic drugs
Surgery
If symptoms persist after medical therapy, then doctors opt for surgical treatment of hypertrophic obstructive cardiomyopathy. The surgical approach to the treatment of HOCM includes septal reduction therapy such as surgical myomectomy and catheter-based alcohol septal ablation.
- Surgical myomectomy is a procedure in which the surgeon simply removes the excess tissue of the hypertrophied ventricle. This removes the obstruction to the left ventricular outflow tract. Some complications can arise after this procedure such as ventricular septal defect (due to excessive removal of the fibrous tissue) and Left ventricular dysfunction (due to damage of myocardial segments during the surgery).
- Alcohol septal ablation is a catheter-based and less invasive procedure in which alcohol (ethanol) is infused in the septal perforator coronary arteries. This results in thrombosis and infarction of the inter-ventricular septum. The infarcted tissue thins and this relieves the outflow tract obstruction.
Results for surgical myomectomy are better than alcohol septal ablation with a 90% success rate. Also, there is a lower risk of cardiovascular complications in surgical myomectomy. Alcohol septal ablation may require a second surgical procedure.
Risk for sudden cardiac death
Most people have a low risk for sudden cardiac death. However, a small number of patients have a higher risk of sudden cardiac death. This includes patients who have:
- History of arrhythmias with a fast heartbeat
- Family history of sudden cardiac death
- Had several episodes of fainting or syncope
- Severe symptoms
- Poor heart function
You can discuss your potential risk with your doctor. He/she might prescribe you preventive measures such as anti-arrhythmic medications or implantable cardioverter-defibrillator.