When bacteria or other infectious organisms spread into the bloodstream it is called septicaemia. The non-medical terminology for septicaemia is ‘blood infection’ or ‘blood poisoning’. It requires hospitalization and treatment with a multidisciplinary medical team.
When the septicaemia causes dangerous and potentially life-threatening symptoms it is called ‘sepsis’. Many people use both terms interchangeably but in reality both are not exactly the same.
Why does it happen?
People with weakened immune systems are more prone to develop septicaemia. There are many causes of weakened immune system, for example:
- AIDS
- Diabetes mellitus
- Cancer
- Advanced age
- Cigarette smoking
- Malnutrition
- Liver cirrhosis
- Side-effects of many medicines e.g. ciclosporin, steroids, cyclophosphamide, chemotherapy drugs etc.
Almost any infection has the potential to reach the bloodstream and cause septicemia. Some of the common infections causing septicaemia are:
- Urinary tract infection (infection in the water system of the body)
- Wound infection
- Infective endocarditis (an infection in the inner layer of the heart)
- Insect/ animal bite
- Tattooing
- Pneumonia
- Appendicitis
- Osteomyelitis (infection in bone)
- Cellulitis
- Peritonitis
- Meningitis (infection in brains’ covering)
- Hospital acquired
In some cases the exact cause of septicaemia cannot be identified.
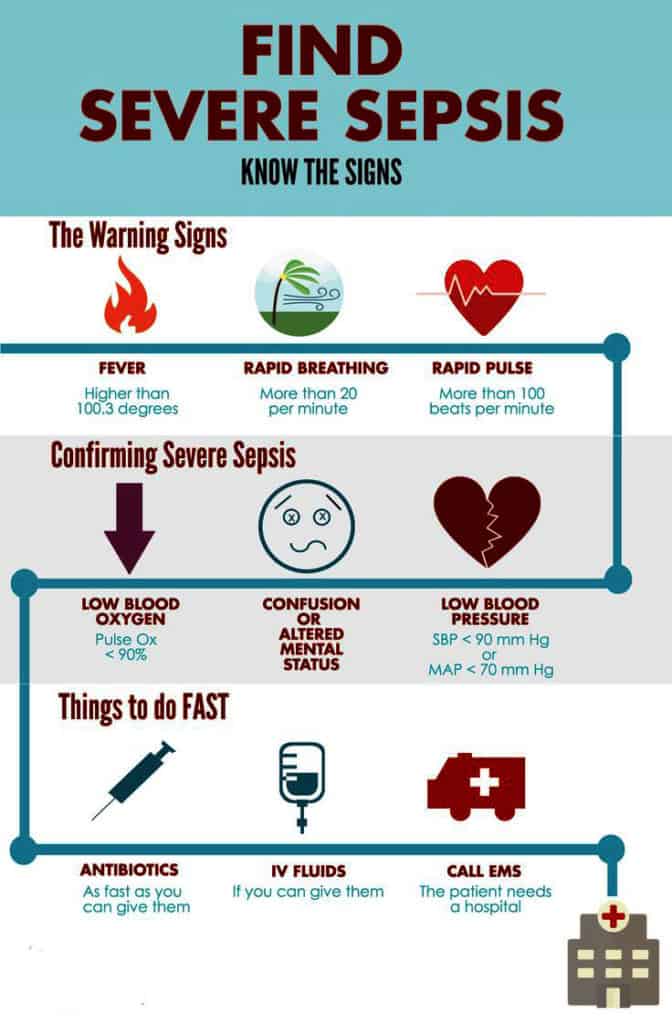
The signs and symptoms of sepsis
The signs and symptoms of sepsis can develop very fast. Therefore, treatment must be started as soon as possible. Some of the common symptoms are:
- Patients may feel very weak and unwell
- Fever
- Chills
- Low blood pressure
- Fast heart rate
- Fast breathing and breathing difficulty
When these symptoms progress then patient can develop septic shock. Features of septic shock are:
- Cold clammy skin
- Very low to unobtainable blood pressure
- Very rapid pulse and heart rhythm disturbance
- Low or no urine output
- Drowsiness or confusion
- Skin rash
- Multi-organ failure due to lack of blood supply to the organs.
- Acute respiratory distress syndrome – a life-threatening acute condition where lungs cannot exchange sufficient amounts of oxygen and carbon dioxide.
- Increased tendency to form blood clots within the blood channels.
How to diagnose it?
Usually, there will be a history of weakened immune systems and/ or infection. Then there would be some signs and symptoms discussed above. The following investigations can be done to formally diagnose it:
- Blood culture – may show growth of bacteria or other microorganisms e.g. viruses or fungus.
- Complete blood count may show an increased amount of neutrophils and white blood cells. Platelet count may also increase because it is an acute phase reactant.
- Wound/ sputum/ urine culture can be given to find out the potential organisms causing sepsis.
- Imaging such as x-ray, CT-scan, MRI, echocardiogram, and ultrasonogram can be done to find out the abscess, vegetations, and infectious foci.
Some other tests can be done to check organ functions and blood coagulability, such as:
- Liver function test
- Renal function test
- Clotting factors assay
- Arterial blood gas analysis
Is sepsis contagious?
Sepsis itself is generally not contagious. But if highly infectious bacteria in blood causes sepsis then it may be contagious to some extent for example clostridium difficile. Therefore protective gears and items of clothing should be worn by the caregivers. And the patient should be isolated from the general wards to prevent infection from spreading to other patients.
Treatment of septic shock
Treatment must never be delayed. Managing sepsis requires intensive care unit support and a multidisciplinary team which includes an internal medicine specialist, blood doctor, heart doctor, ICU nurse, infectious disease specialist, lung doctor and more. Once sepsis is clinically suspected don’t wait for culture results or imaging tests.
- Start antibiotic therapy which covers a broad spectrum of bacteria
- If the viral cause or fungal cause of sepsis is suspected then antivirals and antifungals can also be added
- Maintain airway and give oxygen if oxygen saturation is low
- Proper hydration to maintain blood pressure
- Sometimes steroids can be used to reduce inflammation.
- Medications that increase blood pressure (vasopressors) and prevents cardiac arrhythmia
- Sometimes surgery may be needed to remove the source of infection.
Complications of sepsis
- Multi-organ damage
- Acute respiratory distress syndrome
- Death
Outcome of sepsis
In particular, abdominal sepsis exhibits the highest mortality rate with 72%. The long-term prognosis is equally poor; only approximately 30% survived the first year after hospital admission. For more information you can read this research: Epidemiology and Outcome of Severe Sepsis and Septic Shock in Surgical Intensive Care Units in Northern Taiwan
Conclusion
Even after the massive improvement in medical science the death rate of sepsis remains very high. If you suspect someone has developed signs and symptoms of sepsis then immediately call for medical attention.



