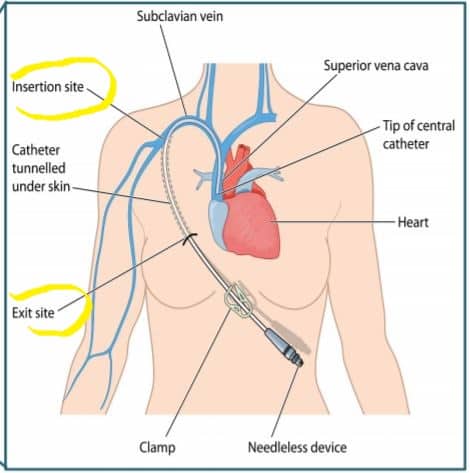
CLABSI- “Central line associated bloodstream infection” is a type of HAI (Hospital Acquired Infection) that occurs through a central venous catheter inserted into the human body provided that the patient had had a central line within 48 hours prior to the development of bloodstream infection. Central Venous Catheter is an intravascular device that is inserted into one of the great vessels of the heart or either the superior or the inferior vena cava when indicated.
Simply, direct entry of organisms through the central vein into the bloodstream causing infection within 48 hours of insertion is known as CLABSI. It is one of the most deadly HAIs.
When and How is the “Central venous catheter” used?
Some of the settings in which the central venous catheterization is done include monitoring of central venous pressure, fluid resuscitation, and emergency venous access in patients with no peripheral access.
Central venous catheterization is a complex procedure. It is placed in one of the crucial places of the human body from where infection can easily enter the body in a very short time.
Hence, the central venous line cannot be frequently changed once it is inserted considering the high chance of bloodstream infection. It is said that unless indicated, a central venous line once inserted should be replaced only after a few weeks or months.
Prevalence of CLABSI
- The prevalence of CLABSI is measured “as the number of infections per 1000 central line-days”.
- According to a report of August 2021, in the United States, the prevalence of CLABSI was found to be 0.8/1000 central line-days. The figure was even higher before that.
- As time passes by, the rate of CLABSI is gradually decreasing in comparison to the past.
Causative Organism
CLABSI is caused by varieties of organisms as a part of HAI. The three most common organisms causing CLABSI in the hospital setting are:
- Coagulase-negative staphylococci.
- Escherichia coli.
- Enterococcus faecium.
Who is at risk of acquiring CLABSI?
The following groups of people when inserted with a central venous line are at high risk of acquiring CLABSI.
- Immunocompromised patients.
- Neutropenic patients.
- Patients with protein calorie malnutrition.
- Patients with severe skin burn.
- Hospitalized for a very long time prior to central line insertion.
Other than these there are some extrinsic risk factors related to the device or insertion sites which can be modified with extra precautions and care.
Sources of infection
The organisms causing CLABSI enter into the body through different sources in and around the central venous catheter, the common sources of infection being;
- The insertion site.
- The connector hub/ The Y part of the catheter.
- Seeding from another source of infection nearby.
- Contaminated infusate.
Among these 95% of the organisms enter from the insertion site and the connector hub portion of the catheter.
Diagnosis
CLABSI is suspected if the patient with a central venous line shows most of the following signs and symptoms:
- Pain, redness or swelling around the central line site
- Pus oozing out from the central line site
- Fever (>38 degree celsius)
- Chills and Rigors
- Respiratory distress
- Altered mental status
- Hypotension
- Bradycardia
All these signs and symptoms in a patient with a central venous catheter inserted in his/her body without any other identifiable source of bloodstream infection are diagnosed as CLABSI.
Other than this, for identification of the proper organism that caused the infection, blood culture is done from blood samples obtained from the central line as well as one from a peripheral vein. This is really important for the treatment purpose as the choice of treatment varies according to the organism.
Treatment
Treatment of CLABSI includes a combination of medical as well as supportive therapy.
Depending upon the organisms found in the blood cultures as well as the severity of the infection, the choice of medicine varies.
CLABSI once diagnosed should always be treated with intravenous antibiotics. Even before diagnosis, empirical antibiotic therapy should be started soon after CLABSI is suspected, keeping in mind the most common organisms that might have caused the infection. The antibiotics can be changed as required after the blood culture reports arrive.
Along with the medical therapy, supportive therapy is equally important in a patient with CLABSI. Supportive treatment includes:
- Intravenous fluid therapy.
- Oxygen therapy when indicated.
- Continuous assessment and monitoring of the vital signs.
- If possible, the central venous catheter should be removed.
Prevention
The prevention strategies for CLABSI can be categorized into four major areas:
- Proper site selection
- Proper hand hygiene
- Proper skin preparation
- Proper barrier precaution
- Proper site selection:
The site for catheter insertion is directly associated with increase or decrease in the risk of acquiring CLABSI. For example: Femoral vein catheterization causes more prone infection than in any other central veins. Hence, selection of site wisely is essential in minimizing the risk of CLABSI.
Likewise, ultrasound-guided catheterization could be done after site selection to reduce the number of attempts, thus reducing the chance of infection.
- Proper hand hygiene:
Cleaning and sanitizing hands is very important before insertion or maintenance of the catheter. After proper cleaning and sanitization, sterile gloves should be worn always before handling the catheter.
This will also help to reduce the chance of developing CLABSI following central venous catheterization to some extent.
- Proper skin preparation:
Standard aseptic measures should be followed while preparing the skin for catheter insertion. This is obtained by the use of alcohol-based chlorhexidine solution. Use of the solution ensures maintenance of proper asepsis.
After cleaning the area with the solution the skin should be let to dry before catheterization.
- Proper barrier precaution:
Along with hand hygiene, one should also maintain as much aseptic precaution as possible of the overall body. For this, proper sterile gowns, caps, masks, etc. should also be worn along with the sterile gloves as far as possible.
Please write your thoughts in the comment section. Here are some other relevant articles for you: