Rheumatic heart disease is a disorder in which rheumatic fever has caused irreversible damage to the heart valves. Shortly after an untreated or inadequately treated streptococcal infection, such as strep throat or scarlet fever, the heart valve damage may manifest. An immune reaction induces an inflammatory state in the body, which can result in permanent valve damage.
Risk factors
Rheumatic fever primarily affects children and adolescents in low- and middle-income countries, particularly those with widespread poverty and inadequate access to health care. Those who reside in overcrowded and impoverished settings are at the greatest risk of contracting the disease.
In regions where rheumatic fever and rheumatic heart disease are endemic, rheumatic heart disease is the leading cause of maternal and perinatal morbidity and mortality in pregnant women. As a result of increased blood volume exerting higher pressure on the heart valves, pregnant women with rheumatic heart disease are at risk for poor outcomes, such as arrhythmias and heart failure. Pregnancy is a common time for women to discover if they have rheumatic heart disease.
Despite having eradicated in many regions of the world, the disease is still prevalent in sub-Saharan Africa, the Middle East, Central and South Asia, the South Pacific, as well as among immigrants and elderly adults in high-income nations, particularly among indigenous populations.
Signs and symptoms
The following are symptoms of rheumatic fever, which can progress to rheumatic heart disease:
- Swelling, inflammation, and joint pain
- An inflammation of the heart muscle and tissue that causes a fast heart rate, tiredness, shortness of breath, and intolerance to exercise
- Fever
- Uncontrollable motions of the limbs
- A rash that is frequently blotchy but rarely itchy
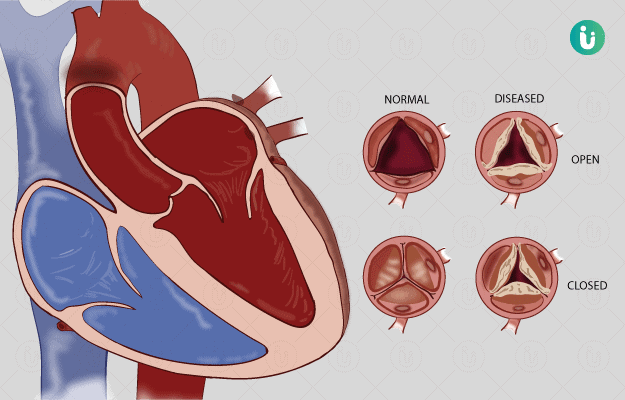
Depending on the severity and location of heart injury, the symptoms of rheumatic heart disease will vary. Heart valve abnormalities can occur from rheumatic heart disease, and their symptoms include:
- Chest pain
- Excessive tiredness
- Cardiac palpitations
- Problems breathing
- Swelling of the ankles, hands, or stomach
- Feeling of beating or thumping in the chest
Diagnosis
No single test exists for rheumatic fever. Rheumatic fever is diagnosed based on a patient’s medical history, physical examination, and test results. Possible rheumatic fever diagnostics include:
Blood testing. Inflammation indicators (markers) in the blood can be detected via blood testing. Included in these tests are C-reactive protein and the erythrocyte sedimentation rate.
- Occasionally, a blood test is performed to discover antibodies to the strep bacterium in the blood. It is possible that the actual germs are no longer detectable in the throat tissue or blood.
- Electrocardiogram (ECG or EKG). This test measures the heart’s electrical activity. It can aid in diagnosing irregular heartbeats and assist a physician identify if portions of the heart are enlarged.
- Echocardiogram. Using sound waves to create images of the heart in motion. An echocardiography depicts the blood flow within the heart and heart valves.
Treatment
Antibiotics are necessary for children with rheumatic fever to combat their strep infection. The physician treating your child may also prescribe anti-inflammatory medication to alleviate joint pain and swelling. Depending on the severity of your child’s condition, they may recommend bed rest for 2 to 12 weeks. After treatment, your kid may need to continue taking medication (prophylactic antibiotics) to prevent a recurrence of the infection.
If your kid experienced rheumatic fever, he or she requires follow-up care with a pediatric cardiologist (heart specialist) to monitor for permanent heart damage. Pediatric cardiologists at the Seattle Youngsters’s Heart Center examine children on a routine basis to detect early symptoms of injury. We provide service for both the prevention and treatment of issues.
A youngster with rheumatic heart disease may be required to take antibiotics for several years to prevent recurrence of rheumatic fever. Recurrent rheumatic fever might cause additional damage to the heart valves.
If your child has a defective heart valve that is narrow or leaks enough blood to strain his or her heart, he or she may require surgery to repair or replace the valve. In certain instances, if the valve is too narrow, surgeons may utilize a catheter treatment (balloon valvuloplasty) to attempt to open the valve without surgery.
Women with rheumatic heart disease who are pregnant
Pregnant women are at heightened risk for rheumatic heart disease. A woman’s blood volume increases during pregnancy. The heart must use more effort to pump the additional blood. During pregnancy, a woman with compromised heart valves may experience major health complications. The health of her unborn child is also at risk.
Complications
These are some complications of rheumatic heart disease:
- Heart failure. This can be caused by a severely constricted or leaking cardiac valve.
- Bacterial endocarditis. This is an infection of the inner lining of the heart, which can arise when the heart valves have been compromised by rheumatic fever.
- Pregnancy and delivery complications owing to heart disease. Before becoming pregnant, women with rheumatic heart disease should discuss their condition with their healthcare professional.
- Valve heart rupture This is a medical emergency that requires immediate heart valve replacement or repair.
Prevention
As rheumatic fever is the cause of rheumatic heart disease, preventing rheumatic fever is an important strategy. The use of proper antibiotics to treat strep throat will avoid rheumatic fever.
Once a patient has been diagnosed as having had rheumatic fever, it is crucial to prevent additional streptococcal infections, which could lead to a recurrence of rheumatic fever and further damage to the heart valves. To prevent additional streptococcal infections, the patient must be treated with antibiotics for an extended period of time. The most successful antibiotic treatment for avoiding subsequent infection is benzathine penicillin G, which is administered intramuscularly every 3 to 4 weeks for many years.
For countries where rheumatic heart disease is endemic, the primary strategies for prevention, control, and elimination are as follows: improving living standards; expanding access to appropriate care; ensuring a consistent supply of quality-assured antibiotics for primary and secondary prevention; and planning, developing, and implementing feasible programs for prevention and control of rheumatic heart disease, supported by adequate monitoring and surveillance, as an integrative approach.



