Brugada syndrome is a rare cardiac rhythm disorder with the potential of causing sudden cardiac death. The heart is usually morphologically and histologically normal in Brugada syndrome.
It is an autosomal dominant disease meaning 50% of the children will inherit it if one parent has it. This syndrome is more commonly seen in Asian people. Men have higher incidence than females. The symptoms of Brugada usually starts at the age of 30 to 40 years. It can cause sudden dangerous heart rhythms like polymorphic ventricular tachycardia and ventricular fibrillation which may be fatal. These dangerous heart rhythms can occur at rest or during sleep. Similar heart rhythms can also be seen in long QT syndrome type 3 (causes arrhythmia at rest or sleep).
Cause
Numerous research has suggested various genetic associations of Brugada. But most research suggests a mutation in the SCN5A gene can cause Brugada syndrome. Normally this gene encodes a subunit of the cardiac voltage-gated sodium channel.
Symptoms
Patients usually have no symptoms. Most of the time they don’t know that they have Brugada syndrome until they experience life-threatening cardiac rhythms. But a few cases can have the following symptoms:
- Racing of heart
- Nocturnal agonal respiration with gasping breath
- Fainting or syncope
- Shortness of breath
ECG findings
The typical ECG findings of the Brugada pattern may not always be present. Certain factors can uncover Brugada pattern in ECG, for example:
- Fever
- Drugs such as beta-blockers, tricyclic anti-depressants, procainamide, and flecainide
- Alcohol and cocaine
In Brugada, the ECG may show pseudo right bundle branch block and ST-segment elevation in V1 to V3.
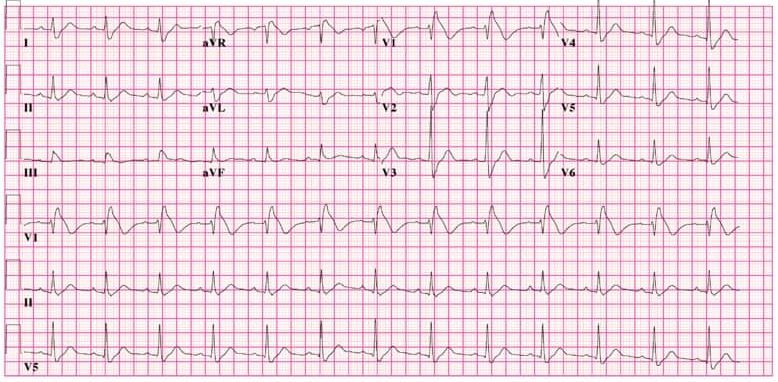
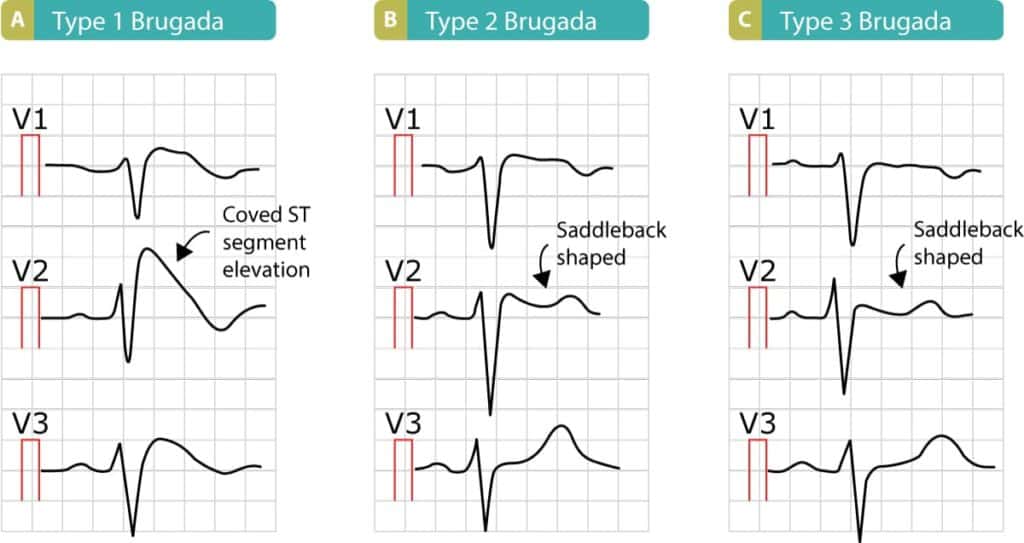
A. Brugada type 1
Elevated ST-segment descending with upward convexity (coved type) to an inverted T-wave.
B. Brugada type 2
Elevated ST-segment descending initially towards the baseline (but remaining 1 or more mm above baseline) and rising again to an upright or biphasic T-wave (saddle back type).
C. Brugada type 3
Similar configuration to type 2, but ST-segment elevation 1 or more mm in type 2 and less than 1 mm in type 3.
Brugada syndrome vs Brugada pattern
- Brugada pattern is the presence of ECG complexes suggestive of Brugada syndrome normally or during provocative testing using flecainide or procainamide.
- Brugada syndrome is the presence of Brugada ECG pattern plus any of the following:
- Polymorphic ventricular tachycardia or ventricular fibrillation
- Unexplained syncope
- Family history of sudden cardiac death at age below 45 years
- Nocturnal agonal respiration
- Any first degree relative diagnosed with type 1 Brugada syndrome
Diagnosis
Brugada syndrome is diagnosed from the patient’s history and ECG patterns. Sometimes sodium channel blockers are administered in the clinic setting to unmask the Brugada pattern in the ECG.
Brugada syndrome treatment
- Patient education and lifestyle advice – avoid sodium channel blockers, and avoid being feverish or hyperthermic.
- Quinidine.
- Implantable cardiac defibrillators.