Tinea unguium is a widespread form of fungal infection. Also known as onychomycosis. The fungus typically attacks the fingernails and toenails. It is more prevalent in men, older adults, and those with weakened immune systems due to diabetes, psoriasis, peripheral vascular disease, or another condition.
Risk factors
- Age and gender: senior citizens and men;
- Environment: wet and damp climate or environment;
- Physical variables include infection history, immunosuppression, and peripheral vascular disease.
Symptoms and Indicators
- Tinea unguium is characterized by white or yellow nail discoloration, nail thickness, and nail detachment from the nail bed. There are four distinct kinds of tinea unguium:
- Distal subungual onychomycosis is the most prevalent form of tinea unguium, which is caused by Trichophyton rubrum on the nail bed or underneath the nail plate.
- White superficial onychomycosis is caused by more than a fungus invasion of the nail plate’s surface layers.
- In immunocompromised patients, proximal subungual onychomycosis is caused by fungal penetration of the freshly formed nail plate through the proximal nail fold.
- Candidal onychomycosis: caused by Candida species, candidal onychomycosis is an infection of the fingernails of individuals who frequently submerge their hands in water.

Diagnosis
- Clinical evaluation
- Examination of potassium hydroxide wet mount
- Biological culture or polymerase chain reaction (PCR)
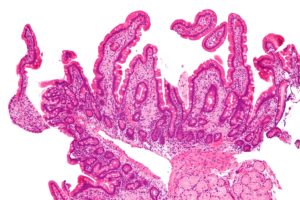
- Histopathologic analysis of nail clippings and subungual detritus stained with periodic acid-Schiff (PAS).
- (See also an update on the current diagnostic and therapeutic techniques for onychomycosis.)
- Onychomycosis is suspected in individuals with tinea pedis based on clinical presentation; predictive clinical symptoms include involvement of the third or fifth toenail, involvement of the first and fifth toenails on the same foot, and unilateral nail deformity. Consider subclinical onychomycosis in patients with recurrent tinea pedis.
- Differentiation from psoriasis or lichen planus is essential because the treatments are distinct; therefore, the diagnosis is often verified by microscopic inspection and, if microscopic findings are inconclusive, culture of scrapings or PCR of clippings. On the afflicted nail, scrapings are obtained from the most proximal accessible location, inspected for hyphae on a potassium hydroxide wet mount, and cultured. Although more expensive, PCR has become an increasingly popular method for confirming the diagnosis of onychomycosis, particularly when cultures are negative or when a conclusive diagnosis is necessary. PAS-stained nail clippings and subungual debris may also be examined histopathologically.
- It can be difficult to obtain a sufficient sample of nails for culture since the distal subungual debris, which is easy to sample, typically does not contain active fungus. Therefore, removing the distal portion of the nail with clippers or using a small curette to get more proximally beneath the nail will boost the yield.
Treatment
- Mild infections involving less than 80 percent of one or two nails may respond to topical antifungal drugs, but oral antifungal medications are typically required for treatment. Infections of the fingernails are typically treated more promptly and efficiently than infections of the toenails.
- Effective medications are costly, and treatment is not always recommended:
- Even if a fungal culture is positive, the nail disease may not be caused by fungus.
- The infection could be symptomless.
- The patient can be unwilling to apply or consume a drug.
- The elderly have an extremely high failure rate.
- Among the adverse effects of antifungal medicines are severe allergic reactions and death
- Interactions between medications can be dangerous.
For nail plate infections, topical antifungals are taken twice weekly for six to twelve months:
- Amorolfine (Loceryl™) nail lacquer
- Ciclopirox (Batrafen™) nail lacquer
- Subsidization for oral azole antifungals requires specialist approval. They are contraindicated during pregnancy. From 6 to 12 weeks (fingernails) or 3 to 6 months (toenails):
- Terbinafine (LamisilTM, TerbinafinTM) 250 mg once daily tablets
- Itraconazole (SporanoxTM) 100 mg capsules, 200 mg once daily, or 200 mg bd for seven days per month
- Rarely is nail removal essential, however, it may be considered in cases of complete nail disintegration. Surgical removal is painful and unpleasant. Chemical evulsion can be accomplished by putting urea paste under occlusion and repeating as needed every few days. Many months may pass before the nail regrows.