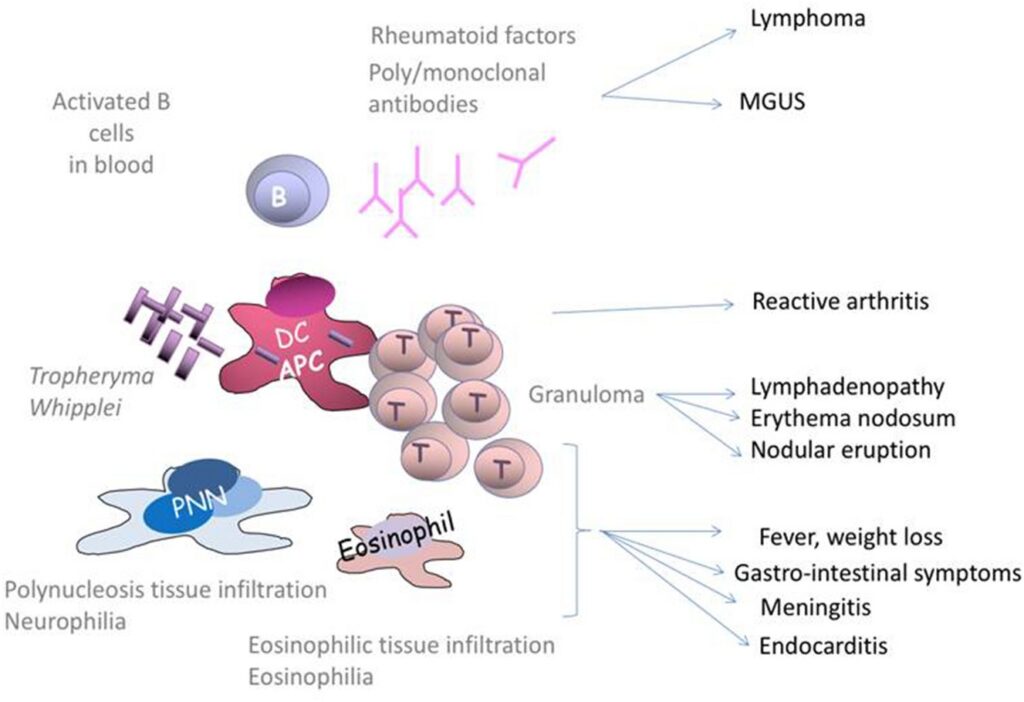
Whipple’s illness is a severe bacterial infection that affects numerous body systems. It is an incredibly rare illness that predominantly affects white men of middle age. Some individuals may have a genetic susceptibility to the condition. Patients report diarrhea, weight loss, abdominal pain, and joint pain as symptoms. The illness is named after George Whipple, who in 1907 documented a patient suffering from it.
Whipple disease cause
The bacterium Tropheryma whipplei causes Whipple illness. Scientists are uncertain as to how T. whipplei infects humans, however, this bacterium appears to be prevalent in soil and water. (It should come as no surprise that many cases of Whipple illness are reported among agricultural and construction workers who have frequent contact with soil.
Diagnosis
- It was not able to diagnose the germs responsible for Whipple until quite recently.
- In 2000, T. Whipplei was successfully recreated in the laboratory. This led to the creation of a straightforward blood test for diagnosing the condition.
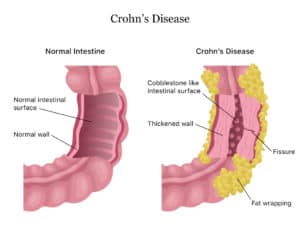
- The presence of Whipple disease’s distinctive intestinal lesions aids in the disease’s diagnosis.
- The best technique to detect these lesions is to do a small intestinal biopsy via upper endoscopy. During the process, a thin, flexible tube is inserted into the esophagus through the mouth.
- Whipple disease is identified endoscopically by patches of enlarged folds with a granular, yellow-white, shaggy covering.
- The polymerase chain reaction (PCR) technique was utilized to identify T. Whipplei-specific DNA in diverse tissue samples from individuals with Whipple disease.
- PCR can confirm a diagnosis of Whipple disease when it cannot be established histologically or by examining tissue under a microscope. PCR has a high degree of sensitivity and specificity, making it beneficial in ambiguous and questionable instances.
- In 1997, researchers hypothesized that a negative PCR result following treatment could be indicative of a low clinical relapse rate. Patients who got treatment but still had a positive PCR result following therapy may be more likely to experience a recurrence, according to their findings.
- Up to fifty percent of patients with Whipple illness have an infection of the central nervous system, but not all show clinical or radiologic manifestations of the disease.
- In these instances, a PCR examination of the cerebral fluid may be beneficial. This may aid in the diagnosis of cerebral Whipple disease.
Whipple disease treatment
- Antibiotics
- Late relapse is a possibility
- Untreated illness is fatal and progressing
Numerous antibiotics (e.g., trimethoprim/sulfamethoxazole, penicillin, cephalosporins) are curative. For 2 to 4 weeks, ceftriaxone (2 g IV daily) or penicillin G (1.5 to 6 million units IV every 6 hours) is used to treat Whipple illness. A long-term course of oral therapy with trimethoprim/sulfamethoxazole (160/800 mg twice daily for 1 year) or a combination of doxycycline (100 mg twice daily for 1 year) and hydroxychloroquine follows this regimen (200 mg 3 times a day for 1 year). Patients with a sensitivity to sulfa may substitute oral penicillin VK or ampicillin. There is a rapid clinical recovery, with fever and joint problems disappearing within a few days. Generally, intestinal symptoms resolve after 1 to 4 weeks.
To confirm therapy response, polymerase chain reaction (PCR) testing on stool, saliva, or other tissue is possible. Other authorities, however, urge a repeat biopsy after one year with microscopy to document bacilli (not simply macrophages, which may survive for years after effective therapy) in addition to PCR testing.
Relapses are common and might occur years after the initial episode. If a relapse is suspected, biopsies of the small intestine or PCR testing should be performed (independent of the organ systems affected) to determine the presence of free bacilli.
Complications
Patients with central nervous system (CNS)–related Whipple illness tend to be more susceptible to relapse.
A response or allergy to antibiotics is a potential problem that could necessitate altering the antibiotic drug.
When should I contact a physician?
You should contact your physician if you experience:
- Issues with balance or coordination
- Chest discomfort or difficulty breathing.
- Joint discomfort.
- Appetite loss or unintentional weight loss
- Seizures.
- Extreme abdominal discomfort or diarrhea
- Problems with vision, speaking or swallowing.
Long-Term Prospects
Within a month of beginning medication, many of the symptoms will have disappeared. The best course of action is to continue taking your medicines. Relapses are common. When they manifest, additional symptoms, such as neurological issues, may also manifest.