Introduction
- Depression, also called Major depressive disorder or clinical depression, is a serious mood disorder causing a prolonged feeling of extreme sadness, low mood, lack of interest, etc. that interferes with everyday activities resulting in lower productivity and some chronic health conditions.
- It is a normal part of life to feel down because sad and mood lowering events happen to everyone from time to time. But, when such feelings occur regularly, and last for at least 2 weeks, then that person could be dealing with depression.
- It is a state of mood in which a person’s emotions such as hopelessness and despair won’t go away and it hampers with the ability to work, study, eat, sleep, and enjoy life.
- Depression is the leading cause of disability in the world.
- Major depressive disorder has significant potential morbidity and mortality due to its high risk of suicidal tendency.
Epidemiology of clinical depression
- Incidence: Around 4-5% of the global population affecting more than 300 million people worldwide, according to the UN World Health Organization (WHO).
- Sex: Women are affected more than men (2:1)
- Age: Young (20-30 years) and the elderly.
Types of depression
American Psychiatric Association classified major depressive disorder into different subtypes referred to as “specifiers.”
- Persistent depressive disorder (Dysthymia): It is a chronic and low-grade depression with mild symptoms that lasts for at least 2 years.
- Atypical depression: It is a type of depression in which a temporary mood lift is experienced in response to some positive events, such as after receiving a good news or while going out with friends and family, etc.
- Psychotic depression occurs when a person has severe depression plus some form of psychosis, such as delusions and hallucinations.
- Seasonal affective disorder is characterized by the onset of depression when there is reduced daylight especially during the winter. Patients generally recover during spring and summer.
- Peripartum depression: It is a depression particularly affecting women during pregnancy, or within 3 months after delivery due to hormonal changes and added responsibilities of a child.
- Melancholic depression: It is associated with deep sadness and despair and loss of pleasure in activities that were once enjoyable.
- Catatonic depression: This type of depression is very rare and serious which involves disturbances of motor behavior and other related symptoms such as the person is usually mute, remains immobile, or shows purposeless or even bizarre movements.

Pathophysiology
The pathophysiology of depression is not yet understood. But there are certain theories such as:
-
Monoamine hypothesis: It includes deficiency of Serotonin, noradrenaline (norepinephrine), and dopamine. Serotonin is a monoamine neurotransmitter which is involved in physiologic activities such as pain sensation, appetite regulation, aggression and mood. Dysfunction in the serotonergic system results in mood and anxiety disorders.
-
Hypothalamic-pituitary-adrenal (HPA) axis: Chronic stress results in hyperactivity of the HPA axis that leads to elevated cortisol levels and affects certain regions of the brain such as amygdala which is responsible for emotional reactivity..
-
Circadian rhythm in depression: A pineal gland hormone named melatonin regulates the rhythm of various biological activities like core temperature, cortisol hormone secretion, and sleep cycles by acting on receptors in hypothalamus. Decreased level of melatonergic signaling in the neurons results in delayed onset of sleep, difficulty in maintaining sleep and early morning awakening, etc.
-
Neurotrophic hypothesis: Depressed patients have low levels of brain-derived neurotrophic factor (BDNF) which is an important molecular regulator of neuronal development important in the learning and adaptation process which seems to be deficient in patients with depression.
Triggering factors of depression
There is no single cause of depression. There are a variety of reasons that trigger depression
- Genetic predisposition: Depression runs in the family
- Stressful life events:
- Death of loved ones
- loss of relationship (such as divorce, breakups) or unhappy relationships
- unemployment
- negligence/feeling unwanted
- Loneliness and isolation
- Physical or Sexual Abuse
- Bullying
- Trauma
- Financial difficulties
- One’s Personality:
- Low self-esteem person easily gets depressed in minor issues
- Rapid mood changes
- Being self-critical
- Alcohol and substance abuse
- Drugs:
- Phenothiazines
- Phenylbutazone
- Corticosteroids
- Oral contraceptives
- Interferon
Medical conditions associated with clinical depression
- Neurological
- After severe stroke
- Multiple sclerosis
- Wilson’s disease
- Traumatic head injury
- Parkinson’s disease
- Huntington’s disease
- Alzheimer’s disease
- Epilepsy
- Heart diseases (such as myocardial infarction etc.)
- Endocrine
- Hypothyroidism and hyperthyroidism
- Cushing’s syndrome / Addison’s disease
- Hyperparathyroidism
- Diabetes Mellitus
- Infections
- Infectious mononucleosis
- HIV
- Herpes simplex
- Neurosyphilis
- Lyme disease
- Hepatitis C
- Toxoplasmosis
- Connective tissue disease
- Malignant diseases
- Stomach or pancreatic cancer
- Paraneoplastic syndrome
- Others:
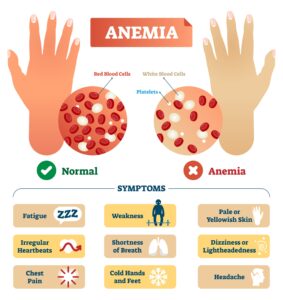
- B12 Deficiency
- Fibromyalgia / Chronic fatigue / chronic pain etc.
Clinical features
- Psychological:
- low mood
- Reduced self-esteem
- Feeling of hopeless and helpless
- Pessimism
- Guilt
- Loss of interest
- Lack of enjoyment (anhedonia)
- Suicidal tendency
- Physical symptoms:
- loss of appetite
- Weight change
- Disturbed sleep
- Fatigue
- Loss of libido
- Bowel disturbance
- Motor retardation (slowing of activity)
- Social symptoms:
- Avoiding contact with friends and family
- Taking part in fewer social activities
- Neglecting hobbies
- Having difficulties at home, work or family life
Diagnosis
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM–5)
Any 5 or more of the 9 symptoms should be present:
- Low mood
- Loss of interest/pleasure in activities
- Significant weight loss/gain
- Sleep disturbances (inability to sleep or oversleeping)
- Psychomotor agitation or impairments
- Fatigue
- A feeling of worthlessness/guilt
- Decrease concentration
- Recurrent thoughts of death or suicidal tendency
Investigations
No specific investigation is required for the diagnosis of depression but it is necessary if there is a suspicion of an underlying medical disorder, such as Cushing’s syndrome or hypothyroidism.
Management
Pharmacological
- Antidepressant drugs:
- Antidepressant drugs are effective in moderate and severe depression.
- The patient’s progress must be monitored and treatment should be continued for at least 6–12 months to reduce the high risk of relapse.
- The dose should then be tapered off over several weeks to avoid discontinuation symptoms.
- Tricyclic antidepressant drugs
- Amitriptyline
- Imipramine
- Dosulepin
- Clomipramine
- Selective serotonin reuptake inhibitors (SSRIs) – they are less cardiotoxic and less sedative than TCAs
- Citalopram
- Escitalopram
- Fluoxetine
- Sertraline
- Paroxetine
- Monoamine oxidase inhibitors- They are now rarely prescribed since they can cause potentially dangerous interactions with drugs such as amphetamines and certain anesthetic agents and with foods rich in tyramine (such as cheese and red wine).
- Phenelzine
- Tranylcypromine
- Moclobemide
- Noradrenaline (norepinephrine) reuptake inhibitors and SSRIs
- Venlafaxine
- Duloxetine
- Lithium
- Mirtazapine
- Antipsychotics
Non-pharmacological
Counseling
- Counseling helps to think about the problems that the patient is experiencing in life so
- that it can help to find new ways of dealing with them.
Psychotherapy
They are based on talking with patients, either individually or in groups It involves emphatic listening to the patient’s condition of their symptoms, their problems, and associated fears and concerns, followed by actively helping them to tackle problems in a structured way.
Benefits of psychotherapy:
- Helps to cope up with a current crisis or other difficult situation
- Identify and correct negative beliefs and behaviors
- Improves relationships and develop positive interactions with others
- Find better ways to face and solve problems
- Identify issues that contribute to depression and change behaviors that make it worse
- Recreate a sense of satisfaction
- Have control over life
- Learn to set realistic goals
- Develop the ability to tolerate stressful situation using healthier behaviors
Types of psychotherapy:
Cognitive behavior therapy aims to help patients to identify cognitive errors such as a tendency to interpret events in a negative way or see them as unduly threatening and to learn how to challenge them as well as assist in changing the unhelpful behavior of the patient, such as anger/suicidal tendency.
Interpersonal therapy
Interpersonal psychotherapy (IPT) focuses on the interpersonal relationships of the patient.
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) produces a convulsion by brief administration of a high-voltage direct-current impulse to the brain in an anesthetized and paralyzed patient in order to boost the function and effect of neurotransmitters in the brain to relieve depression. It is usually safe, proven to be effective in case of severe depressive illness with few side-effects, if properly given.
Indication of ECT:
- not improving with medications.
- Cannot take antidepressants for health reasons.
- High risk of suicide.
Transcranial magnetic stimulation (TMS) or deep transcranial magnetic stimulation is a noninvasive method used to stimulate small regions of the brain.
Light therapy can help regulate mood and improve symptoms of depression and is commonly used in seasonal affective disorder.
Additional therapies
- Acupuncture
- Relaxation techniques such as yoga or meditation
- Massage therapy
- Music or art therapy
- Herbal supplements
- St. John’s wort
- SAMe,
- Omega-3 fatty acid
Prevention
It is believed that the mind and body must be in harmony for us to stay healthy. Some lifestyle modifications and technique that will help to achieve such harmony and prevent depression are:
- Love and support from family and friends
- Having a strong social network – reach out to people and share feelings
- Motivation
- Avoid alcohol and substance abuse
- Eat healthily – drink plenty of water, eat fruits, and vegetables
- Physical activities – walking, jogging, swimming, gardening, or another activity that you enjoy.
- Get plenty of sleep. Having proper sound sleep is important for both physical and mental well-being.
- Proper education about depression
Prognosis
- 70-80% of individuals with clinical disorder show a significant reduction in the intensity of symptoms and the frequency of episodes if appropriate treatment is given. Many people recover quickly while some may not respond to the initial treatment.
- After complete recovery, there is a 40% risk of relapse, hence the patient should be under the consultation with the psychiatrist for maintenance therapy.
- If symptoms have not fully resolved with appropriate treatment then there is a chance of recurrence or being chronic. Sometimes, people need to take lifelong medications to control their symptoms.