Cancer is not a singular illness. There are numerous forms of cancer. However, all cancers begin when a group of cells in the body proliferate uncontrollably. Cancer cells continue to proliferate and might force out healthy cells. This makes it difficult for the body to function properly. Cancer can begin in any part of the body. It can originate in the breast, lungs, colon, and even the blood. Cancer that originates in the lungs is known as lung cancer. Cancer cells are capable of spreading to other organs. For example, lung cancer cells can move to the bone and flourish there. The spread of cancer cells is known as metastasis. Cancer is always called after the origin of the disease. Therefore, when lung cancer spreads to the brain (or elsewhere), it is still referred to as lung cancer. It is not referred to as brain cancer unless it originates in the brain.
Small cell lung carcinoma is the rarest kind of lung cancer, yet it spreads more quickly than non-small cell lung cancer. Screenings for lung cancer can discover small cell lung cancer before it spreads, when the disease is most amenable to treatment using procedures such as radiation therapy, immunotherapy, and chemotherapy.
Types
There are two primary kinds:
- Small-cell carcinoma (oat cell cancer)
- Combined small-cell carcinoma
Both include several cell types that develop and spread in distinct ways. They are named based on how the cells appear under a microscope.
Small cell vs non-small cell cancers
In the following ways, small-cell lung cancer differs from non-small-cell lung cancer:
- The growth of small-cell lung carcinoma is rapid.
- The spread of small-cell lung carcinoma is rapid.
- Chemotherapy (using drugs to kill cancer cells) and radiation therapy are effective against small-cell lung cancer (using high-dose X-rays or other high-energy rays to kill cancer cells).
- Different paraneoplastic disorders are commonly associated with small-cell lung cancer (a collection of symptoms that result from substances produced by the tumor).
Symptoms
SCLC is typically asymptomatic, meaning it does not produce symptoms. Once symptoms manifest, it is usually a sign that the cancer has spread to other parts of the body.
Typically, the severity of symptoms increases as the cancer grows and spreads.
Possible symptoms include:
- Bloody phlegm in the lungs
- Problems breathing
- Wheezing
- Chest discomfort or pain
- Chronic coughing or hoarseness
- A diminished appetite
- Weight loss
- Fatigue
- Facial enlargement
Call your doctor immediately if any of these symptoms are present. It may not be SCLC, but if it is, it is important to detect it early.
Causes
SCLC is mostly caused by carcinogens (chemicals that cause cancer) found in cigarette smoke. These carcinogens cause DNA (deoxyribonucleic acid; genes) damage in cells, resulting in cancer. However, it is unknown why exactly normal cells turn malignant. Multiple variables, including genetic and environmental ones, undoubtedly contribute to the development of SCLC in certain individuals. Current research reveals that anomalies in DNA, the genetic code carrier of the body, are the underlying cause of malignant transformation of cells.
Oncogenes or tumor suppressor genes may be impacted by genetic alterations in SCLC. These gene modifications are acquired throughout life and are not inherited. They are acquired from exposure to environmental variables, such as smoking, or they arise at random for unknown causes (spontaneously). Normal genes that control cell development and division are changed or missing in these genes. A mutated oncogene encourages unrestrained growth (cancer). Typically, tumor suppressor genes restrict or stop the proliferation of cells. When tumor suppressor genes are defective, cells can grow uncontrollably, leading to cancer. When normal genes are present, they appear to inhibit the development of cancer.
Multiple oncogenes and tumor suppressor genes have been related to small cell lung cancer (SCLC). The TP53 gene, which has been connected to many cancers, and the RB1 gene, which has been linked to retinoblastoma and other malignancies, are two tumor suppressor genes that have been linked to numerous cases of SCLC. The TP53 gene is mutated in 75% of SCLCs, whereas the RB1 gene is mutated in 90% of SCLCs.
Multiple risk factors are related with SCLC. A risk factor is something that enhances an individual’s likelihood of developing a disease. Possessing a risk factor does not guarantee that a person will get a condition, and those without risk factors can nevertheless develop a condition. Over 95 percent of SCLC patients are current or past smokers, making smoking the primary risk factor for the disease. Heavy smokers are especially susceptible to SCLC. Additionally, secondhand smoke exposure raises the risk of lung cancer. Less frequent environmental risk factors include exposure to chloromethyl esters, which are used in the production of chemicals, asbestos, or radon. Radon is a radioactive, odorless, and colorless gas. Uranium dioxide occurs naturally in the environment when uranium decomposes in soil or rock. Concentrated radon exposure, which can sometimes occur within a home, typically in the basement, can raise the chance of developing lung cancer.
Diagnostic testing
Tests may consist of:
- Imaging testing. Your pulmonary X-ray may detect an abnormal lump or nodule. A CT scan can detect tiny lung lesions that may not be visible on an X-ray.
- Sputum cytology. Examining sputum produced by a coughing individual under a microscope can sometimes indicate the presence of lung cancer cells.
- Tissue sample (biopsy). A biopsy is a technique in which an aberrant cell sample is extracted.
- Your doctor can do a biopsy in a variety of techniques, including bronchoscopy, in which a lighted tube is put down your neck and into your lungs to check abnormal parts of your lungs.
- Mediastinoscopy, in which an incision is created at the base of the neck and surgical instruments are introduced beneath the breastbone to obtain lymph node tissue samples, is also a possibility.
- Needle biopsy is another possibility, in which your physician uses X-ray or CT pictures to guide a needle through your chest wall and into your lung tissue in order to collect abnormal cells.
- Lymph nodes or other places where the cancer has spread, such as the liver, may also be biopsied.
- A laboratory examination of your cancer cells will identify the sort of lung cancer you have. The precise properties of your cells, as revealed by modern testing, can help your doctor determine your prognosis and direct your treatment.
- Tests to identify the cancer’s extent.
Tests to establish the cancer's extent
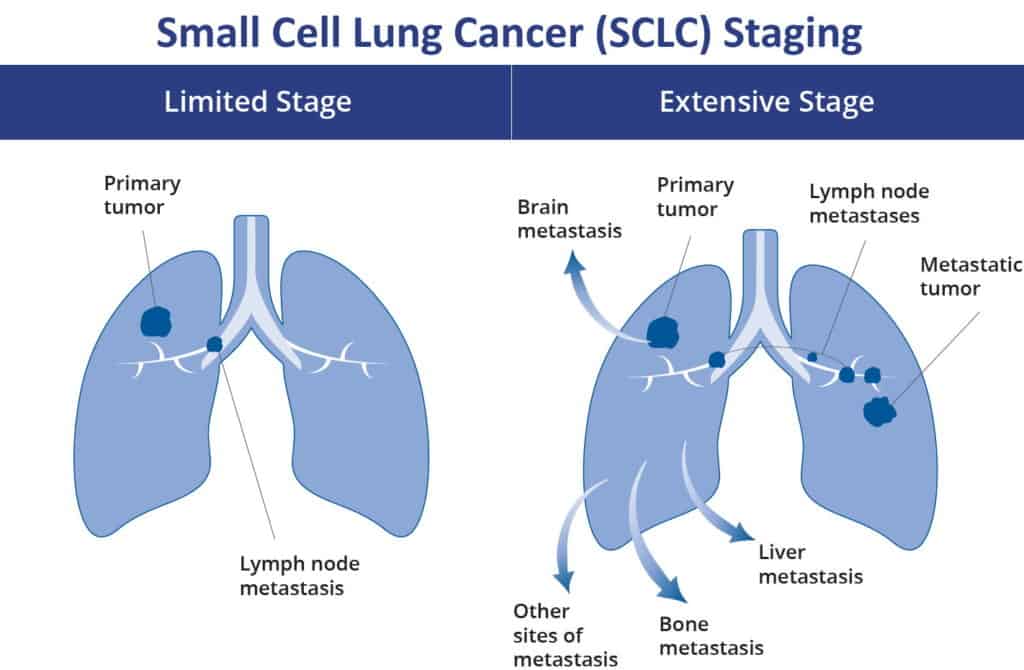
After a lung cancer diagnosis has been made, your doctor will establish the extent (stage) of the disease. The stage of your cancer helps you and your doctor determine the most appropriate treatment.
Your doctor may use imaging treatments to see if your cancer has spread beyond your lungs during staging. These examinations include computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), and bone scans. Not every test is appropriate for every individual; therefore, you should discuss with your doctor whether treatments are appropriate for you.
The stages of lung cancer are denoted by Roman numerals ranging from 0 to IV, with the lower stages denoting lung-confined malignancy. The cancer is considered advanced and has spread to other parts of the body at stage IV.
Stages
The stage of a cancer describes its size, location, and spread from its original site. Knowing the stage allows your doctors to recommend the most effective treatment for you.
Small cell lung cancer and non-small cell lung cancer share the same staging method. Using a staging scale ranging from 1 to 4, your physician may describe the stage of your lung cancer.
The staging considers:
- The size of the malignancy
- If the cancer has progressed to neighboring lung tissue or beyond the lung
- If the cancer has spread to local lymph nodes, lymph nodes in the chest, or lymph nodes further distant, the patient will undergo surgery.
- If the cancer has progressed to other areas of the body or beyond the lungs.
- The staging also considers whether the lung has partially or completely collapsed.
The majority of number steps are subdivided. In an attempt to maintain simplicity, we have omitted these. Your doctor or nurse can provide more information about the stage of your lung cancer.
Treatment options
Lung cancer is treated in a variety of methods, depending on the kind and extent of the disease. Surgery, chemotherapy, radiation therapy, targeted therapy, or a combination of these treatments may be used to treat non-small cell lung cancer. Typically, radiation treatment and chemotherapy are used to treat small cell lung cancer.
- Surgery. A surgery in which cancerous tissue is surgically removed.
- Chemotherapy. Utilizing specialized drugs to shrink or eradicate the cancer. The drugs may be administered orally or intravenously, or sometimes both.
- Radiation treatment. Utilizing similar to X-rays high-energy radiation to eradicate cancer.
- Targeted treatment. Utilizing medications to inhibit the development and spread of cancer cells. The drugs may be taken orally or administered intravenously. Before this treatment is administered, tests will be performed to determine whether targeted therapy is appropriate for your kind of cancer.
Doctors from various specialities frequently collaborate to treat lung cancer. Pulmonologists are physicians who specialize in lung illnesses. Surgeons are doctors who perform surgical procedures. Thoracic surgeons specialize in surgery of the chest, heart, and lungs. Medical oncologists are physicians who use medications to treat cancer. Radiation oncologists are physicians who use radiation to treat malignancies.
Prognosis
Sixty to seventy percent of patients with small cell lung cancer (SCLC) present with clinically disseminated or widespread illness. SCLC at its extensive stage is incurable. Patients with extensive-stage cancer who get combination chemotherapy had a full response rate of more than 20 percent and a median survival of more than 7 months; nevertheless, just 2 percent remain alive after 5 years. A complete response rate of 80 percent and a survival rate of 17 months have been recorded for patients with limited-stage disease treated with a combination of chemotherapy and chest radiation; 12 to 15 percent of patients are still alive after five years.
Genome-wide association studies have found single-nucleotide polymorphisms (e.g., in the promoter region of YAP1 on chromosome 11q22) that may influence the longevity of SCLC patients.
Among the indicators of a poor prognosis are the following:
- Disease relapse
- Weight reduction exceeding 10 percent of initial body weight
- Poor overall performance
- Hyponatremia