Barrett’s esophagus is a disorder in which squamous cells, the normal cells that line the esophagus, transform into specialized columnar cells, which are not typically found in humans. This condition is known as intestinal metaplasia because the specialized columnar cells resemble the gut lining. Damage to the esophageal lining leads the cells to alter. Less than 1 percent of individuals with this disease develop esophageal cancer. However, Barrett’s esophagus may raise the chance of esophageal cancer development.
Cell level changes in Barrett's Esophagus
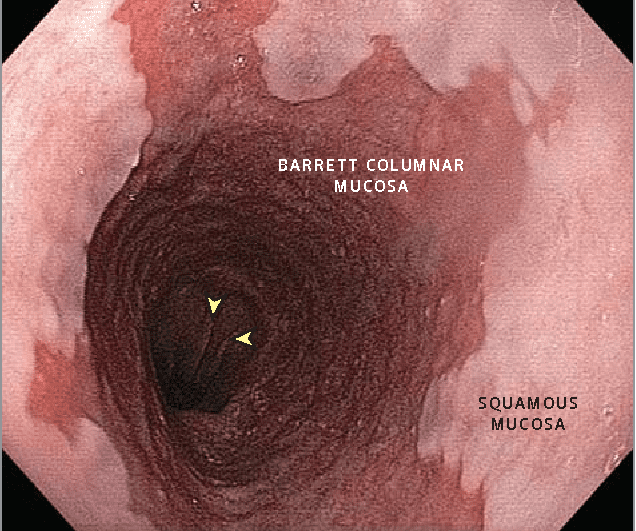
A healthy esophagus is coated with pinkish-white, flat, smooth cells (squamous cells) that allow food to pass easily. The stomach lining is composed of towering red cells that secrete an acid-resistant mucus. The cells lining the esophagus become inflamed and irritated by refluxed food, gastric juices, and (potentially) bile because they are not acid-resistant. The ensuing discomfort is referred to as heartburn.
Without therapy, chronic exposure to these liquids might cause cellular alterations in the lower esophagus. The flat smooth cells are replaced with the red mucus-secreting cells commonly found in the stomach. Red cells in the esophagus are indicative of Barrett’s esophagus.
Symptoms of Barrett's Esophagus
Although Barrett’s esophagus does not generate symptoms, it is possible for a patient to develop gastroesophageal reflux disease symptoms (GERD). These consist of:
- Burning pain in the chest (heartburn)
- Food regurgitation or the sensation of acid burning in the esophagus or mouth
- Difficulties swallowing
- Chest pain that is not caused by a heart issue
- There is a lump in the neck
- Undiagnosed nausea
- Coughing, hoarseness or wheezing
Risk factors
Diagnosis
- To diagnose Barrett’s esophagus, healthcare providers may offer an endoscopy for patients with acid reflux symptoms. This involves inserting a thin, flexible tube with a light at the end to examine the esophagus, stomach, and intestines.
- Endoscopy is used to search for particular alterations in the esophageal lining that may indicate Barrett’s esophagus.
- Endoscopy will be used to monitor a patient after the diagnosis has been made. These frequently occur:
- After one year, then every three years if no tissue alterations are seen.
- Six to twelve months after diagnosis for patients with moderate tissue changes
- The physician may collect a tissue sample, often known as a biopsy, concurrently. Typically, this will be performed under minimal sedation.
- It is difficult for physicians to obtain a biopsy of the complete esophageal lining. Not all regions contain Barrett’s. Consequently, the doctor will normally perform at least eight biopsies throughout the process.
- Normal tissue appears differently than Barrett’s tissue. The appearance of normal tissue is pale and glossy, whereas Barrett’s tissue is red and velvety.
Treatment
Barrett esophagus should be treated similarly to GERD, although most sources agree that a proton pump inhibitor (PPI) should be used instead of an H2-receptor antagonist due to the significant acid insensitivity of Barrett esophageal patients. Despite the fact that PPIs are more effective than H2-receptor antagonists at reducing stomach acid output, it remains unclear whether PPIs promote regression of Barrett esophagus.
Higher levels of esophageal tissue alterations caused by Barrett’s esophagus typically do not manifest until adulthood. Depending on the severity of dysplasia, doctors may employ treatments such as:
- Endoscopic resection (using an endoscope to remove damaged cells)
- Electromagnetic ablation (using heat to remove abnormal tissue)
- Frost therapy (using extreme cold to remove abnormal tissue)
- Surgical removal of the affected esophageal segment
Barrett’s esophagus can reoccur despite treatment, especially if the underlying cause of chronic inflammation is not treated.
How to prevent Barrett's esophagus?
The most critical stage is minimizing and reducing acid reflux. Effective strategies include:
- If you are overweight and obese, lose weight.
- Don’t smoke
- Limit alcohol consumption
- Consume smaller meals and delay bedtime by a few hours
- Avoid late-night snacking
- Sleep with your head slightly elevated (nighttime GERD is more destructive because the esophagus is also “sleeping” and is unable to force acid down immediately).
- Avoid chocolate, coffee, peppermint, fatty or spicy foods as well as tomatoes and tomato-based goods.



