Bronchopneumonia is an infection of the lower respiratory tract characterized by widespread inflammation throughout the lungs. This form of pneumonia is primarily observed in youngsters and is caused by bacteria.
Bronchopneumonia is typically caused by a bacterial infection, but it can also be brought on by viral or fungal infections. Pathogens such as Staphylococcus aureus, Klebsiella pneumoniae, Hemophilus influenzae, Streptococcus pneumoniae, Pseudomonas aeruginosa, and Escherichia coli can cause bronchopneumonia. Other, less frequent species that can cause pneumonia include viruses like SARS-Cov-2 and fungus like Aspergillus fumigatus.
Bronchopneumonia is characterized by suppurative inflammation that is concentrated around the bronchi and may affect one or more lung lobes. In extreme situations, bronchopneumonia might result in the development of a lung abscess (pus-filled pocket in a focal area). This disorder is also known as empyema.
Symptoms
Bronchopneumonia symptoms may resemble those of other kinds of pneumonia. This disorder typically begins with flu-like symptoms that might worsen over several days. Among the symptoms are:
- fever
- a cough which produces mucous
- Insufficiency of breath
- chest pain
- fast respiration
- sweating
- chills
- headaches
- muscular aches
- pleurisy, or chest pain caused by inflammation resulting from excessive coughing
- fatigue
- bewilderment or delirium, particularly in the elderly
People with compromised immune systems or other disorders may experience very severe effects.
Causes
The most prevalent reasons:
- A bacterial lung infection, such as Streptococcus pneumoniae and Haemophilus influenza type b, is the Trusted Source of bronchopneumonia (Hib). Viruses and fungi are also capable of causing pneumonia.
- Infectious organisms can enter the bronchi and alveoli and begin to proliferate. Inflammation is caused by the immune system’s production of white blood cells that assault these pathogens. Frequently, symptoms result from this inflammation.
Among the risk factors for bronchopneumonia are:
- being under 2 years of age
- being at least 65 years old
- usage of tobacco or excessive alcohol
- Recent respiratory diseases, including the cold and influenza
- COPD, cystic fibrosis, bronchiectasis, and asthma are examples of chronic lung illnesses.
- additional medical issues, including diabetes, heart failure, and liver disease
- HIV and certain autoimmune illnesses are immune-system-weakening conditions.
- Taking medicines that suppress the immune system, such as chemotherapy, organ transplantation, or prolonged steroid use.
- recent surgery or accident
Diagnosis
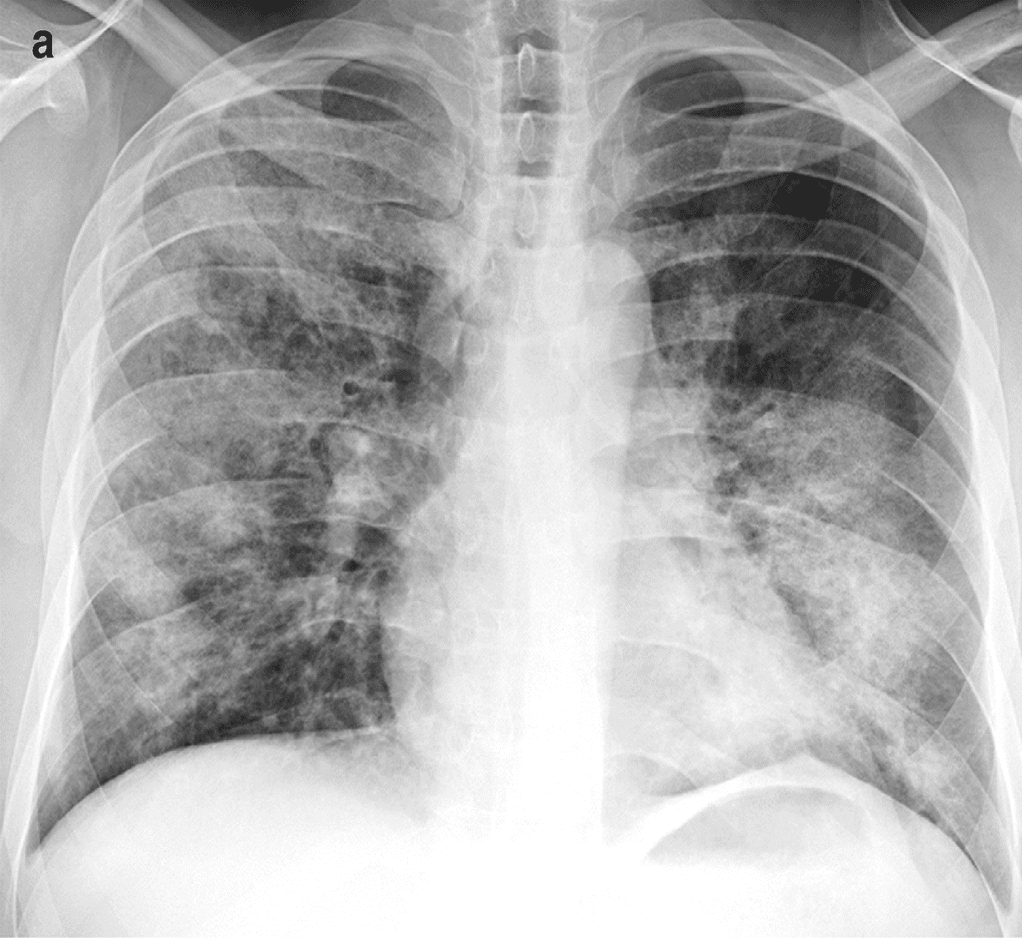
The clinical diagnosis of bronchopneumonia is based on your symptoms and chest X-ray results.
The diagnosis of bronchopneumonia always begins with a comprehensive clinical history and a focused physical exam, including stethoscope examination of the heart and lungs for wheezing and other abnormal breathing sounds.
Blood tests searching for symptoms of infection, such as a complete blood cell count (CBC), and chest X-rays may be conducted initially.
On chest X-rays, bronchopneumonia typically appears as one or more patchy consolidations involving one or more lobes (sections of the lungs). Inflammation and its byproduct (neutrophilic exudates) are typically localized in the bronchi (air passages in the lungs) and bronchioles (smaller air passages that branch off from the bronchi), and then spread to the neighboring alveoli (tiny air sacs). 1
In addition, utilizing pulse oximetry and an arterial blood gas test, your oxygen levels and oxygen flow throughout your body will be evaluated.
If you come with a productive cough (coughing up mucus), a sputum culture may be conducted to examine mucus for symptoms of bacterial infection.
In addition, your healthcare professional may perform a bronchoscopy, which involves sending a tiny tube with a light and camera down your windpipe and into your lungs. This looks for evidence of infection and suspicious spots warranting further study via biopsy (removing sample tissue for examination in the lab).
Treatment
- The treatment for pneumonia varies on the kind of pneumonia, the causative pathogen, and the severity of the infection.
- Antibiotics are effective against bacterial and certain fungal pneumonias. They are ineffective against viral pneumonia.
- In some circumstances, your clinician may prescribe antiviral drugs for viral pneumonia
- Other kinds of fungal pneumonia are treated with antifungals.
- If your symptoms are severe or you are at risk for consequences, hospitalization may be necessary. You may receive additional treatments there. If your blood oxygen level is low, for instance, you may receive oxygen therapy.
- There may be a delay in recovery from pneumonia. Some individuals recover within a week. For some, it may take a month or longer.
Complications
Occasionally, pneumonia can result in grave complications such as:
- The condition of bacteremia, which occurs when bacteria enter the bloodstream. It is a dangerous condition that can result in septic shock.
- Lung abscesses are pus-filled formations in the cavities of the lungs.
- Pleural diseases are disorders that affect the pleura. The pleura is the tissue that lines the interior of the chest cavity and covers the exterior of the lungs.
- Renal failure
- respiratory incapacity
Prognosis
The prognosis for bronchopneumonia is generally favorable, but relies on a number of variables, including:
- Age
- Medical history
- Hospital setting
- Typically, if you are normally healthy, your symptoms will resolve within one to three weeks after receiving treatment.
- The majority of instances of bronchopneumonia can be treated with rest, antibiotics administered outside of the hospital, and routine follow-up.