Cauda equina syndrome (CES) is a rare but serious condition where nerves at the bottom of the spinal cord become compressed. Because these nerves control sensation and function in the legs, bladder, bowel, and sexual organs, CES is a medical emergency. Getting urgent assessment and treatment can reduce the risk of permanent nerve damage.
This article explains what CES is, the warning signs, what to do, and what to expect during diagnosis and treatment.
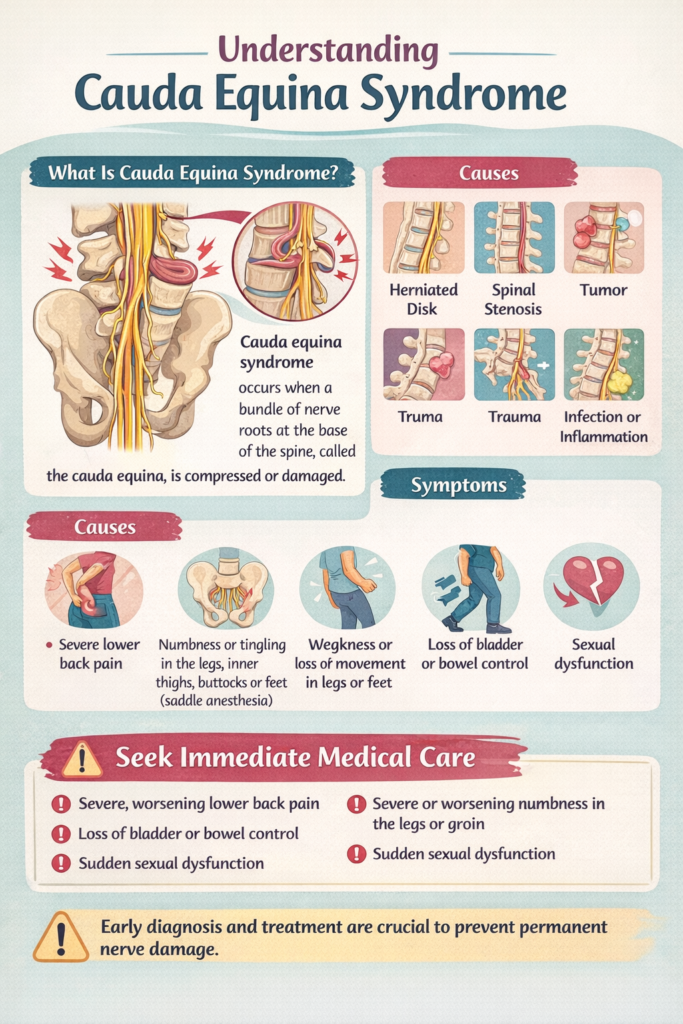
What is cauda equina syndrome?
At the lower end of your spinal cord, the nerves spread out in a bundle that looks a bit like a horse’s tail—this bundle is called the cauda equina (“horse’s tail” in Latin). These nerves send signals to and from the:
- Legs and feet
- Bladder and bowel
- Genital area and sexual function
Cauda equina syndrome happens when these nerves are squeezed or damaged, often suddenly, causing symptoms that can become permanent if not treated quickly.
What causes cauda equina syndrome?
CES is usually caused by something that takes up space and presses on the nerves in the lower spine. Common causes include:
- Large slipped (herniated) disc in the lower back
- Spinal stenosis (narrowing of the spinal canal), sometimes with a sudden worsening
- Injury/trauma to the spine
- Tumor pressing on nerves
- Infection or inflammation around the spine
- Bleeding (hematoma) after surgery or procedures (less common)
Most people who get CES have severe nerve compression and need urgent assessment.
Key warning signs and symptoms
Back pain and sciatica are common problems and do not usually mean CES. What makes CES different is the combination of symptoms—especially changes in bladder/bowel control or numbness in the “saddle area.”
Red flag symptoms (seek emergency care)
Call emergency services or go to the emergency department immediately if you develop any of the following, especially if they are new or worsening:
- Trouble passing urine (difficulty starting, weak stream, or feeling unable to empty your bladder)
- New loss of bladder control (incontinence)
- Loss of bowel control or new stool leakage
- Numbness/tingling in the saddle area
(the area that would touch a saddle: inner thighs, groin, genitals, buttocks) - New weakness in one or both legs, difficulty walking, or foot drop
- Severe, worsening lower back pain, often with sciatica on one or both sides
- New sexual dysfunction (such as reduced sensation)
If you’re unsure but have bladder changes or saddle numbness, it’s safer to treat it as urgent.
Why is cauda equina syndrome an emergency?
Nerves can be permanently damaged if they are compressed for too long. Permanent problems may include:
- Ongoing bladder or bowel difficulties
- Persistent numbness in the groin/saddle area
- Weakness in the legs or feet
- Sexual function changes
- Chronic pain
Early diagnosis and treatment improve the chances of recovery.
What should I do if I suspect CES?
- Do not wait to see if it gets better.
- Seek emergency medical attention now.
- If symptoms are severe or rapidly worsening, call emergency services.
- If possible, tell the clinician clearly:
- “I have new bladder/bowel changes” and/or
- “I have numbness in the saddle area” and/or
- “I have new leg weakness.”
While waiting for care
- Avoid driving yourself if symptoms are severe, you feel weak, or you’re at risk of falling.
- Don’t take extra medication beyond what’s prescribed to “push through”—it can mask changes that matter to clinicians.
How is cauda equina syndrome diagnosed?
In the emergency department or urgent clinic, the team may:
- Ask detailed questions about bladder, bowel, and sensation changes
- Check strength, reflexes, and sensation in your legs and pelvic area
- Sometimes check your bladder after urinating (to see if urine is being retained)
Imaging (usually MRI)
The main test is an MRI scan of the lower spine because it shows whether the nerves are being compressed.
If MRI isn’t immediately available or isn’t safe for you, a different scan may be used depending on the situation.
How is cauda equina syndrome treated?
Treatment depends on the cause, but urgent treatment is often needed.
Surgery (common)
If CES is caused by strong nerve compression (for example, a large disc herniation), doctors may recommend urgent spinal surgery to relieve pressure on the nerves.
Other treatments
If the cause is something else, treatment might include:
- Antibiotics (for infection)
- Steroids or other medicines (for inflammation in selected cases)
- Treatment directed at a tumor (specialist care)
Your care team will explain what applies to your specific situation.
What is recovery like?
Recovery varies widely. Some people improve quickly after treatment, while others recover gradually over months. Possible outcomes include:
- Improved leg pain and strength (often improves sooner)
- Bladder/bowel function may take longer and may not fully return
- Some people need help from:
- Physiotherapy
- Pelvic health specialists
- Bladder/bowel specialists
- Pain management teams
Follow-up appointments and rehabilitation are common.
Frequently asked questions
“I have sciatica—does that mean I have CES?”
Not usually. Sciatica is common and is most often caused by a disc irritation without CES. CES is more likely when sciatica comes with bladder/bowel changes or saddle numbness.
“If I can still walk, could it still be CES?”
Yes. CES can start with subtle symptoms. Bladder changes and saddle numbness are particularly important even if you can still walk.
“Is CES always sudden?”
Often it develops quickly, but sometimes symptoms build over days. Either way, new bladder/bowel changes are urgent.
Key takeaways
- Cauda equina syndrome is a medical emergency.
- Seek emergency care immediately for new bladder/bowel changes, saddle numbness, or leg weakness.
- Diagnosis usually requires an MRI scan.
- Prompt treatment can reduce the risk of permanent nerve problems.

Leave a Reply